Costochondritis causes inflammation of the cartilage connecting ribs to the breastbone, resulting in sharp chest pain often mistaken for a heart attack. Understanding the symptoms and treatment options is essential for managing discomfort and preventing recurrence. Explore the rest of this article to learn how you can effectively identify and address costochondritis.
Table of Comparison
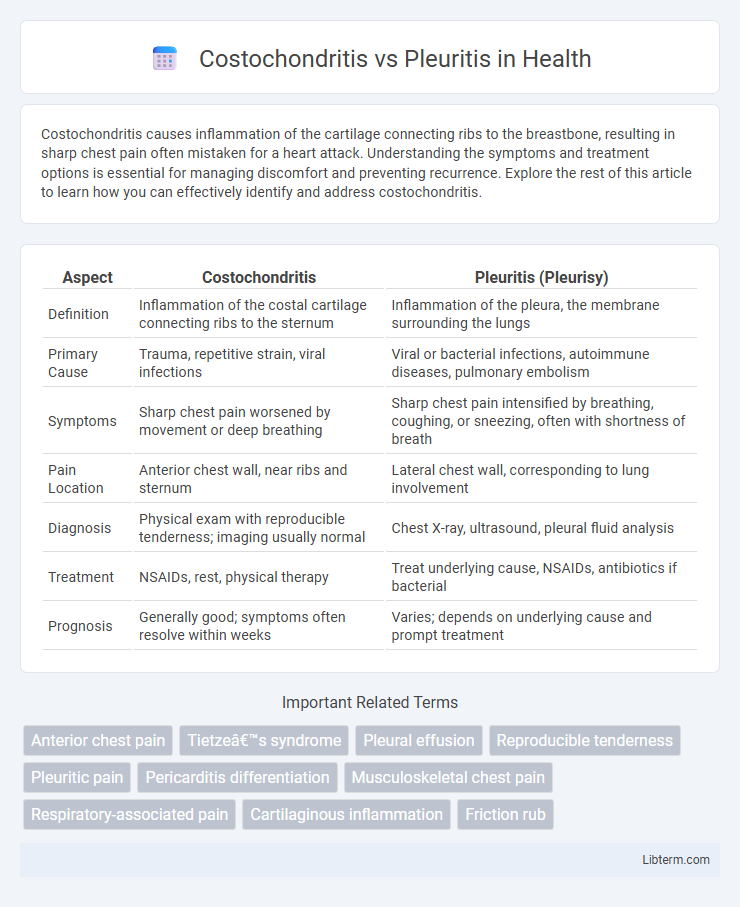
| Aspect | Costochondritis | Pleuritis (Pleurisy) |
|---|---|---|
| Definition | Inflammation of the costal cartilage connecting ribs to the sternum | Inflammation of the pleura, the membrane surrounding the lungs |
| Primary Cause | Trauma, repetitive strain, viral infections | Viral or bacterial infections, autoimmune diseases, pulmonary embolism |
| Symptoms | Sharp chest pain worsened by movement or deep breathing | Sharp chest pain intensified by breathing, coughing, or sneezing, often with shortness of breath |
| Pain Location | Anterior chest wall, near ribs and sternum | Lateral chest wall, corresponding to lung involvement |
| Diagnosis | Physical exam with reproducible tenderness; imaging usually normal | Chest X-ray, ultrasound, pleural fluid analysis |
| Treatment | NSAIDs, rest, physical therapy | Treat underlying cause, NSAIDs, antibiotics if bacterial |
| Prognosis | Generally good; symptoms often resolve within weeks | Varies; depends on underlying cause and prompt treatment |
Introduction to Costochondritis and Pleuritis
Costochondritis is an inflammation of the cartilage connecting the ribs to the sternum, causing localized chest pain that worsens with movement or pressure. Pleuritis, or pleurisy, involves inflammation of the pleura, the membrane surrounding the lungs, leading to sharp chest pain that intensifies during breathing or coughing. Differentiating these conditions relies on understanding their distinct anatomical locations and symptom triggers.
Understanding Chest Pain: Key Differences
Costochondritis causes localized chest pain due to inflammation of the costal cartilage, often tender to touch and worsened by movement or palpation. Pleuritis involves inflammation of the pleura surrounding the lungs, resulting in sharp, stabbing pain that intensifies with deep breaths or coughing. Differentiating these conditions relies on clinical examination and imaging, as costochondritis pain is musculoskeletal while pleuritis pain is respiratory-related.
Causes of Costochondritis
Costochondritis is primarily caused by inflammation of the cartilage connecting the ribs to the breastbone, often resulting from repetitive trauma, heavy lifting, or viral infections. It differs from pleuritis, which is inflammation of the pleura, the membrane surrounding the lungs, typically caused by infections, autoimmune diseases, or pulmonary embolism. Understanding the inflammatory origin of costochondritis is crucial for accurate diagnosis and treatment compared to pleuritis, which has a different etiology and clinical presentation.
Causes of Pleuritis
Pleuritis, also known as pleurisy, is primarily caused by infections such as viral, bacterial, or fungal pathogens that inflame the pleural membranes surrounding the lungs. Other causes include pulmonary embolism, autoimmune diseases like lupus or rheumatoid arthritis, and chest trauma that leads to irritation of the pleura. Unlike costochondritis, which arises from inflammation of the cartilage connecting ribs to the sternum, pleuritis involves direct inflammation of the pleural tissue itself.
Signs and Symptoms Comparison
Costochondritis typically presents with localized chest wall pain that worsens with movement or palpation, often without respiratory symptoms, while pleuritis causes sharp, stabbing chest pain that intensifies during deep breathing or coughing and may be accompanied by shortness of breath or fever. Both conditions result in chest discomfort, but costochondritis pain is musculoskeletal and reproducible by palpation, whereas pleuritis pain is pleuritic and linked to inflammation of the pleura. Diagnosing these conditions relies on distinguishing the physical exam findings and associated respiratory signs characteristic to each.
Diagnostic Methods for Each Condition
Costochondritis diagnosis primarily relies on physical examination revealing localized chest wall tenderness and pain reproducible by palpation, with imaging such as X-rays or MRI typically used to rule out other causes. Pleuritis diagnosis involves chest auscultation detecting pleural friction rubs, chest X-rays to identify pleural effusion or inflammation, and may include ultrasound or CT scans for detailed assessment. Both conditions can require laboratory tests like inflammatory markers, but pleuritis often demands sputum cultures or pleural fluid analysis when infection or malignancy is suspected.
Treatment Options for Costochondritis
Costochondritis treatment primarily involves nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen to reduce inflammation and alleviate pain, with physical therapy and gentle stretching exercises aiding recovery. In severe cases, corticosteroid injections may be administered to decrease localized inflammation, while rest and avoiding activities that exacerbate chest pain are essential. Unlike pleuritis, which may require antibiotics if caused by infection, costochondritis is managed with symptomatic relief and supportive care focused on musculoskeletal inflammation.
Treatment Strategies for Pleuritis
Treatment strategies for pleuritis primarily involve addressing the underlying cause, such as bacterial infections, with appropriate antibiotics or antiviral medications. Pain management is crucial, often utilizing nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids to reduce inflammation and discomfort. In severe cases with pleural effusion, thoracentesis may be necessary to drain excess fluid and alleviate symptoms.
Prevention and Risk Factors
Costochondritis primarily results from repetitive chest wall trauma or viral infections, with risk factors including strenuous physical activity and respiratory illnesses. Pleuritis often associates with underlying lung infections, autoimmune diseases, or pulmonary embolism, increasing risk in individuals with chronic respiratory conditions or immune system disorders. Preventing costochondritis involves avoiding chest injury and managing infections early, whereas preventing pleuritis focuses on controlling lung diseases and reducing exposure to respiratory pathogens.
When to Seek Medical Attention
Severe or worsening chest pain, difficulty breathing, or associated fever with costochondritis or pleuritis requires immediate medical evaluation to rule out life-threatening conditions like myocardial infarction or pulmonary embolism. Persistent chest discomfort lasting more than a few days, especially if accompanied by swelling or tenderness over the ribs, necessitates consultation with a healthcare professional for accurate diagnosis and appropriate treatment. Sudden onset of sharp, localized chest pain exacerbated by breathing or movement signals the need for urgent medical attention to prevent complications such as pleural effusion or chronic inflammation.
Costochondritis Infographic
 libterm.com
libterm.com