Sarcoidosis and lung cancer can present with overlapping symptoms and radiographic findings, making accurate diagnosis crucial for effective treatment. Differentiating between these conditions often requires advanced imaging, biopsy, and careful clinical evaluation to avoid misdiagnosis and ensure appropriate management. Explore the full article to understand the key differences, diagnostic challenges, and treatment approaches for these complex diseases affecting your lungs.
Table of Comparison
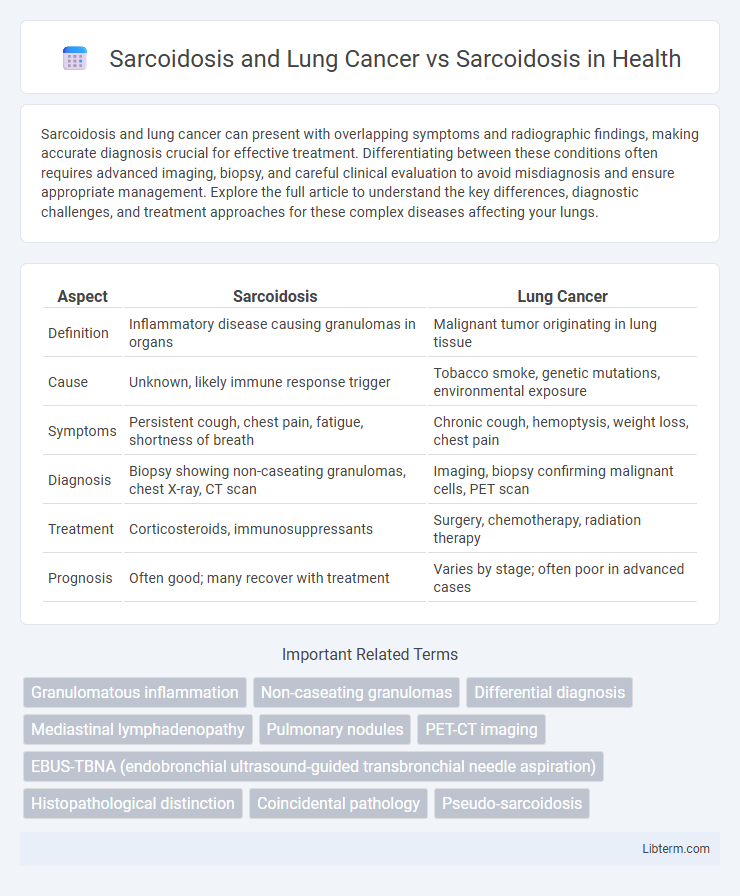
| Aspect | Sarcoidosis | Lung Cancer |
|---|---|---|
| Definition | Inflammatory disease causing granulomas in organs | Malignant tumor originating in lung tissue |
| Cause | Unknown, likely immune response trigger | Tobacco smoke, genetic mutations, environmental exposure |
| Symptoms | Persistent cough, chest pain, fatigue, shortness of breath | Chronic cough, hemoptysis, weight loss, chest pain |
| Diagnosis | Biopsy showing non-caseating granulomas, chest X-ray, CT scan | Imaging, biopsy confirming malignant cells, PET scan |
| Treatment | Corticosteroids, immunosuppressants | Surgery, chemotherapy, radiation therapy |
| Prognosis | Often good; many recover with treatment | Varies by stage; often poor in advanced cases |
Understanding Sarcoidosis: An Overview
Sarcoidosis is an inflammatory disease characterized by the formation of granulomas, primarily affecting the lungs, skin, and lymph nodes. Differentiating sarcoidosis from lung cancer is critical because both can present with similar pulmonary symptoms and imaging findings, yet they require distinct treatments. Advanced diagnostic techniques, including biopsy and PET scans, help accurately distinguish sarcoidosis from malignant lung tumors, ensuring appropriate patient management.
What is Lung Cancer? Key Differences from Sarcoidosis
Lung cancer is a malignant tumor characterized by uncontrolled cell growth in lung tissues, often caused by smoking, genetic factors, or environmental exposures. Unlike sarcoidosis, which is a non-cancerous inflammatory disease causing granulomas in multiple organs, lung cancer involves invasive and destructive growth leading to tissue damage and metastasis. Key differences include lung cancer's cellular malignancy and aggressive progression versus sarcoidosis's immune-mediated granulomatous inflammation, often with a more benign or self-limiting course.
Epidemiology: Sarcoidosis vs Lung Cancer
Sarcoidosis predominantly affects adults aged 20 to 40 years, with an incidence rate of 10 to 20 cases per 100,000 population annually, showing higher prevalence among African Americans and Northern Europeans. Lung cancer, significantly more common in individuals over 65, exhibits an incidence rate of approximately 60 cases per 100,000 population per year, strongly associated with smoking history. Epidemiological data highlight that while sarcoidosis often presents in younger, non-smoking populations, lung cancer primarily impacts older adults with risk factors including tobacco use and environmental exposures.
Shared Risk Factors and Distinct Causes
Sarcoidosis and lung cancer both share exposure to environmental toxins such as cigarette smoke and airborne pollutants, which contribute to lung inflammation and damage. Sarcoidosis primarily stems from an abnormal immune response causing granuloma formation, while lung cancer results from genetic mutations triggering uncontrolled cell growth. Although both diseases affect lung tissue, sarcoidosis is an inflammatory condition, whereas lung cancer is a malignant neoplasm with distinct molecular and pathological mechanisms.
Clinical Presentation: Symptoms Comparison
Sarcoidosis and lung cancer share overlapping clinical presentations such as persistent cough, shortness of breath, and chest pain, complicating differential diagnosis. Sarcoidosis often presents with systemic symptoms including fatigue, fever, and weight loss, whereas lung cancer more commonly involves hemoptysis and localized chest discomfort. Imaging findings and histopathological examination remain critical for accurately distinguishing between granulomatous inflammation characteristic of sarcoidosis and malignant neoplastic lesions seen in lung cancer.
Diagnostic Challenges: Sarcoidosis vs Lung Cancer
Differentiating sarcoidosis from lung cancer remains a significant diagnostic challenge due to overlapping radiologic features such as pulmonary nodules and lymphadenopathy. Histopathological evaluation, including biopsy with granuloma identification for sarcoidosis and malignant cell detection for lung cancer, is essential for accurate diagnosis. Advanced imaging techniques like PET scans can show hypermetabolic activity in both conditions, thus biopsy remains the definitive method to distinguish between sarcoidosis and lung malignancies.
Imaging Findings: Differentiating Features
Imaging findings in sarcoidosis typically reveal bilateral hilar lymphadenopathy and diffuse pulmonary nodules with a perilymphatic distribution, contrasting lung cancer which often presents as a solitary pulmonary nodule or mass with irregular borders and possible cavitation. High-resolution computed tomography (HRCT) in sarcoidosis shows upper lobe-predominant fibrosis and nodular opacities along bronchovascular bundles, while lung cancer imaging may demonstrate spiculated lesions and lymph node enlargement localized to the tumor region. Positron emission tomography (PET) scans can show increased uptake in both conditions, but the pattern of uptake is more diffuse in sarcoidosis versus focal and intense in malignancy, aiding in differentiation.
Biopsy and Histopathology: Confirming the Diagnosis
Biopsy and histopathology play critical roles in distinguishing sarcoidosis from lung cancer by analyzing tissue samples for granulomas characteristic of sarcoidosis versus malignant cells indicative of lung cancer. Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is commonly used to obtain lymph node biopsies, providing high diagnostic yield with minimal invasiveness. Histopathological examination reveals non-caseating granulomas in sarcoidosis, while lung cancer biopsies show cellular atypia and tumor morphology essential for confirming malignancy.
Treatment Approaches: Sarcoidosis and Lung Cancer
Treatment approaches for sarcoidosis primarily involve corticosteroids like prednisone to reduce inflammation and immune system activity, while lung cancer treatment depends on the cancer stage and may include surgery, chemotherapy, radiation therapy, immunotherapy, or targeted therapy. Managing sarcoidosis requires monitoring organ involvement and adjusting immunosuppressive medications accordingly, whereas lung cancer treatment focuses on tumor removal and controlling metastasis. Early diagnosis and tailored treatment plans are crucial for optimizing patient outcomes in both sarcoidosis and lung cancer.
Prognosis and Outcomes: What Patients Should Know
Sarcoidosis and lung cancer differ significantly in prognosis and outcomes, with sarcoidosis often showing spontaneous remission or manageable chronic inflammation, while lung cancer typically requires aggressive treatment due to its potentially fatal nature. Patients diagnosed with sarcoidosis generally experience a favorable prognosis, as the disease primarily affects lung tissue without malignant transformation, whereas lung cancer prognosis depends heavily on the stage at diagnosis, histological subtype, and response to therapy. Understanding these distinctions helps patients anticipate treatment strategies and long-term health impacts, emphasizing the importance of accurate diagnosis and regular monitoring.
Sarcoidosis and Lung Cancer Infographic
 libterm.com
libterm.com