Hemochromatosis is a genetic disorder causing excessive iron accumulation in your body, leading to organ damage if untreated. Managing iron levels through regular monitoring and treatment is crucial to prevent complications such as liver disease, diabetes, and heart problems. Explore the rest of this article to understand symptoms, diagnosis, and effective treatment options for hemochromatosis.
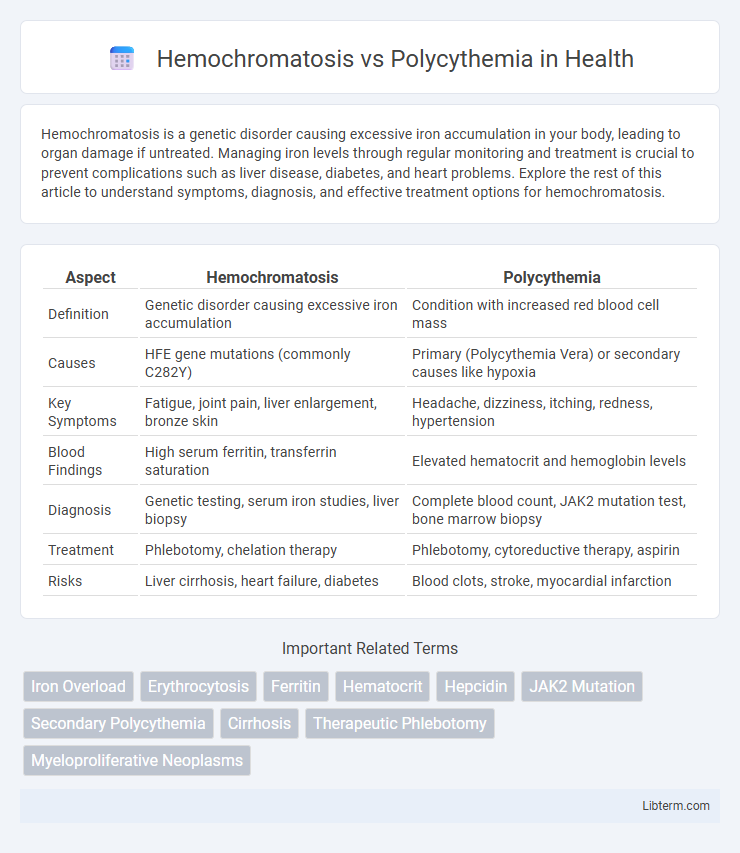
Table of Comparison
| Aspect | Hemochromatosis | Polycythemia |
|---|---|---|
| Definition | Genetic disorder causing excessive iron accumulation | Condition with increased red blood cell mass |
| Causes | HFE gene mutations (commonly C282Y) | Primary (Polycythemia Vera) or secondary causes like hypoxia |
| Key Symptoms | Fatigue, joint pain, liver enlargement, bronze skin | Headache, dizziness, itching, redness, hypertension |
| Blood Findings | High serum ferritin, transferrin saturation | Elevated hematocrit and hemoglobin levels |
| Diagnosis | Genetic testing, serum iron studies, liver biopsy | Complete blood count, JAK2 mutation test, bone marrow biopsy |
| Treatment | Phlebotomy, chelation therapy | Phlebotomy, cytoreductive therapy, aspirin |
| Risks | Liver cirrhosis, heart failure, diabetes | Blood clots, stroke, myocardial infarction |
Overview of Hemochromatosis
Hemochromatosis is a genetic disorder characterized by excessive iron absorption and accumulation in body tissues, leading to organ damage such as liver cirrhosis, diabetes, and heart disease. Unlike polycythemia, which involves increased red blood cell production, hemochromatosis primarily affects iron metabolism and storage. Early diagnosis through serum ferritin and transferrin saturation tests is crucial for effective management and prevention of complications.
Overview of Polycythemia
Polycythemia is a condition characterized by an increased concentration of red blood cells in the bloodstream, leading to elevated hematocrit levels and blood viscosity. It can be classified as primary, such as polycythemia vera caused by JAK2 gene mutations, or secondary due to chronic hypoxia or erythropoietin-secreting tumors. Unlike hemochromatosis, which involves iron overload and tissue damage, polycythemia primarily affects oxygen transport and circulatory dynamics, increasing the risk of thrombosis and stroke.
Key Differences in Pathophysiology
Hemochromatosis involves excessive iron absorption and accumulation in organs, leading to tissue damage and impaired function, primarily caused by genetic mutations affecting iron regulation. Polycythemia is characterized by increased red blood cell mass due to abnormal proliferation of erythroid precursors in the bone marrow, often driven by mutations such as JAK2 V617F. The pathophysiology of hemochromatosis centers on iron overload affecting multiple organs, while polycythemia centers on elevated blood viscosity and risk of thrombosis due to increased red cell volume.
Genetic and Acquired Causes
Hemochromatosis is primarily caused by genetic mutations in the HFE gene, leading to excessive iron absorption and accumulation, with some cases resulting from mutations in other genes like HJV or TFR2. Polycythemia can be classified into primary, often driven by acquired mutations such as JAK2 V617F in polycythemia vera, and secondary forms caused by external factors like chronic hypoxia or tumors producing erythropoietin. Understanding the distinct genetic and acquired causes aids in differentiating these disorders, guiding targeted diagnostic and therapeutic approaches.
Clinical Manifestations Compared
Hemochromatosis primarily presents with symptoms related to iron overload, including fatigue, joint pain, liver cirrhosis, diabetes mellitus, and skin hyperpigmentation. Polycythemia manifests with increased red blood cell mass leading to headaches, dizziness, hypertension, erythromelalgia, and risk of thrombosis due to hyperviscosity. Both conditions can cause fatigue, but hemochromatosis involves metabolic complications while polycythemia affects blood viscosity and oxygen delivery.
Diagnostic Criteria and Laboratory Markers
Hemochromatosis diagnosis primarily relies on elevated serum ferritin levels, increased transferrin saturation above 45%, and genetic testing for HFE gene mutations, particularly C282Y homozygosity. In contrast, polycythemia is characterized by elevated hemoglobin concentration above 16.5 g/dL in men or 16 g/dL in women, increased hematocrit exceeding 49% in men or 48% in women, and often JAK2 V617F mutation analysis to confirm polycythemia vera. Laboratory markers for hemochromatosis focus on iron overload parameters, while polycythemia diagnosis centers on red blood cell mass and bone marrow proliferative markers.
Potential Complications and Risks
Hemochromatosis can lead to severe complications such as liver cirrhosis, diabetes mellitus, heart arrhythmias, and increased risk of hepatocellular carcinoma due to excessive iron accumulation. Polycythemia raises the risk of thrombosis, including deep vein thrombosis, pulmonary embolism, and stroke, as elevated red blood cell mass increases blood viscosity and impairs circulation. Both conditions require careful management to prevent organ damage and life-threatening vascular events.
Treatment Strategies for Each Condition
Hemochromatosis treatment primarily involves regular phlebotomy to reduce iron overload, while iron chelation therapy is used in cases where phlebotomy is contraindicated. Polycythemia vera management centers on phlebotomy to decrease hematocrit levels, alongside low-dose aspirin and myelosuppressive agents like hydroxyurea to control excessive red blood cell production. Both conditions require ongoing monitoring to prevent complications such as organ damage in hemochromatosis and thrombotic events in polycythemia.
Prognosis and Long-term Outcomes
Hemochromatosis prognosis improves significantly with early diagnosis and regular phlebotomy, reducing iron overload and preventing organ damage, while untreated cases often progress to liver cirrhosis, diabetes, or heart failure. Polycythemia, particularly Polycythemia Vera, carries risks of thrombosis and transformation to myelofibrosis or acute leukemia, with prognosis depending on hematocrit control and symptom management. Long-term outcomes in both conditions benefit from continuous monitoring and tailored treatments, but hemochromatosis generally offers a more favorable prognosis if managed before irreversible complications develop.
Frequently Asked Questions (FAQs)
Hemochromatosis causes excessive iron accumulation in tissues, leading to organ damage, while polycythemia results in increased red blood cell production, thickening the blood and raising clot risk. Common questions include how these conditions are diagnosed, with hemochromatosis detected via serum ferritin and transferrin saturation tests, and polycythemia through elevated hemoglobin and hematocrit levels. Treatment queries often focus on phlebotomy for both, yet hemochromatosis requires iron removal, whereas polycythemia aims to reduce blood viscosity and prevent thrombosis.
Hemochromatosis Infographic
 libterm.com
libterm.com