Constipation occurs when bowel movements become infrequent or difficult, often caused by insufficient fiber intake, dehydration, or lack of physical activity. Understanding effective dietary changes and lifestyle adjustments can significantly improve your digestive health and prevent discomfort. Discover practical tips and solutions in the rest of this article to relieve and prevent constipation.
Table of Comparison
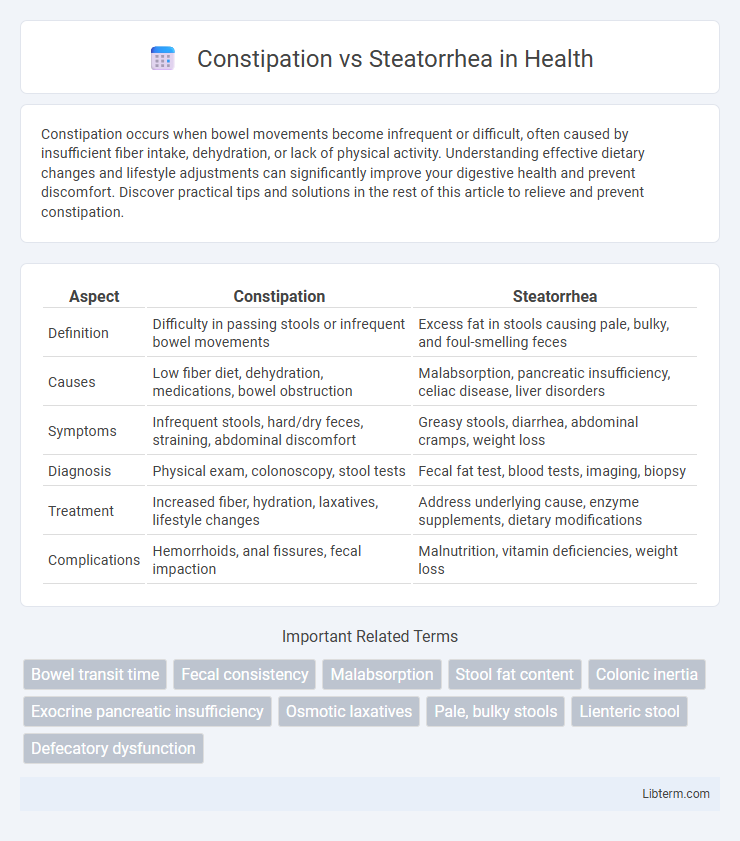
| Aspect | Constipation | Steatorrhea |
|---|---|---|
| Definition | Difficulty in passing stools or infrequent bowel movements | Excess fat in stools causing pale, bulky, and foul-smelling feces |
| Causes | Low fiber diet, dehydration, medications, bowel obstruction | Malabsorption, pancreatic insufficiency, celiac disease, liver disorders |
| Symptoms | Infrequent stools, hard/dry feces, straining, abdominal discomfort | Greasy stools, diarrhea, abdominal cramps, weight loss |
| Diagnosis | Physical exam, colonoscopy, stool tests | Fecal fat test, blood tests, imaging, biopsy |
| Treatment | Increased fiber, hydration, laxatives, lifestyle changes | Address underlying cause, enzyme supplements, dietary modifications |
| Complications | Hemorrhoids, anal fissures, fecal impaction | Malnutrition, vitamin deficiencies, weight loss |
Understanding Constipation: Definition and Causes
Constipation is characterized by infrequent, difficult, or painful bowel movements typically involving hard and dry stools. Common causes include inadequate fiber intake, dehydration, lack of physical activity, certain medications such as opioids, and underlying medical conditions like hypothyroidism or irritable bowel syndrome. Understanding these factors helps differentiate constipation from steatorrhea, which involves oily, foul-smelling stools caused by malabsorption of fats.
Steatorrhea Explained: Meaning and Underlying Factors
Steatorrhea refers to the presence of excess fat in stools, characterized by bulky, pale, and foul-smelling feces that may float due to malabsorption of dietary fats. This condition often indicates underlying disorders such as chronic pancreatitis, celiac disease, or cystic fibrosis, which impair fat digestion or absorption in the gastrointestinal tract. Diagnostic evaluation typically includes stool fat tests, imaging studies, and assessment of pancreatic enzyme function to identify the root cause and guide appropriate treatment.
Key Differences Between Constipation and Steatorrhea
Constipation is characterized by infrequent, difficult, or painful bowel movements due to slowed colonic transit or obstruction, whereas steatorrhea involves abnormal fat excretion in stools, resulting in bulky, greasy, and foul-smelling feces due to malabsorption. Constipation often presents with hard, dry stools and a sensation of incomplete evacuation, while steatorrhea is marked by pale, oily stools that float on water and are resistant to flushing. Diagnostic evaluation for constipation focuses on bowel transit time and obstruction causes, whereas steatorrhea assessment emphasizes pancreatic function, bile acid deficiency, or intestinal mucosal disorders.
Common Symptoms: How They Manifest
Constipation commonly presents with infrequent, hard, and difficult-to-pass stools, often accompanied by abdominal discomfort and bloating. Steatorrhea is characterized by bulky, foul-smelling, greasy stools that float due to high fat content, frequently causing abdominal cramps and malnutrition signs. Both conditions affect bowel habits but differ significantly in stool appearance and underlying digestive issues.
Diagnostic Approaches for Constipation and Steatorrhea
Diagnostic approaches for constipation include a thorough patient history, physical examination, and stool frequency assessment, often supplemented by anorectal manometry and colon transit studies to evaluate bowel function and motility. Steatorrhea diagnosis relies on quantitative fecal fat analysis, typically requiring a 72-hour stool collection, along with pancreatic function tests such as fecal elastase and imaging studies like abdominal CT or MRI to identify malabsorption causes. Distinguishing between constipation and steatorrhea hinges on targeted diagnostic tests assessing bowel motility versus fat malabsorption, guiding appropriate clinical management.
Associated Risk Factors and Medical Conditions
Constipation is commonly linked to risk factors such as low dietary fiber intake, dehydration, sedentary lifestyle, and certain medications like opioids or anticholinergics, with medical conditions including hypothyroidism, diabetes, irritable bowel syndrome, and colorectal cancer contributing to its development. Steatorrhea is associated with malabsorption disorders like chronic pancreatitis, celiac disease, cystic fibrosis, and bile acid deficiency, often resulting from pancreatic enzyme insufficiency or bile duct obstruction. Both conditions signal underlying gastrointestinal dysfunctions requiring targeted diagnostic evaluation to identify specific etiologies and guide effective treatment.
Dietary Influences on Constipation vs Steatorrhea
Dietary fiber intake significantly influences constipation by promoting regular bowel movements and stool softening, whereas steatorrhea is primarily affected by fat malabsorption and inadequate pancreatic enzyme activity rather than fiber consumption. High-fat diets exacerbate steatorrhea by increasing fat content in the stool, while low fiber and fluid intake contribute to slowed intestinal transit and hard stools characteristic of constipation. Adequate hydration supports stool bulk in constipation, whereas enzyme supplementation may be necessary to manage the fatty stools seen in steatorrhea.
Effective Treatment Options for Each Condition
Effective treatment for constipation includes increasing dietary fiber intake, adequate hydration, and regular physical activity to stimulate bowel movements, along with the use of laxatives like osmotic or stimulant types when necessary. Steatorrhea treatment targets the underlying causes such as pancreatic enzyme replacement therapy for pancreatic insufficiency or bile acid supplements for malabsorption syndromes, combined with dietary modifications including low-fat intake. Both conditions require tailored interventions addressing specific pathophysiological mechanisms to achieve symptom relief and improve gastrointestinal health.
When to Seek Medical Help: Warning Signs
Seek medical help for constipation if experiencing severe abdominal pain, persistent vomiting, or inability to pass stool or gas for more than three days. In cases of steatorrhea, medical attention is crucial when fatty, foul-smelling stools persist, are accompanied by weight loss, or signs of malabsorption such as nutrient deficiencies or chronic diarrhea. Early diagnosis and treatment of these warning signs can prevent complications related to underlying gastrointestinal disorders.
Preventive Measures and Long-Term Management
Effective preventive measures for constipation include increasing dietary fiber intake, maintaining adequate hydration, and engaging in regular physical activity to promote bowel motility. Long-term management may involve the use of stool softeners or laxatives under medical supervision and addressing underlying conditions such as irritable bowel syndrome or hypothyroidism. For steatorrhea, prevention focuses on managing malabsorption disorders through enzyme replacement therapy, dietary modifications like reducing fat intake, and monitoring nutrient deficiencies to avoid complications.
Constipation Infographic
 libterm.com
libterm.com