Gout and pseudogout are both forms of arthritis characterized by sudden, intense joint pain caused by crystal deposits, but gout results from uric acid crystals while pseudogout is caused by calcium pyrophosphate crystals. Understanding the differences in symptoms, causes, and treatments is essential for effective management and pain relief. Explore the full article to learn how you can distinguish between these conditions and find the best care options.
Table of Comparison
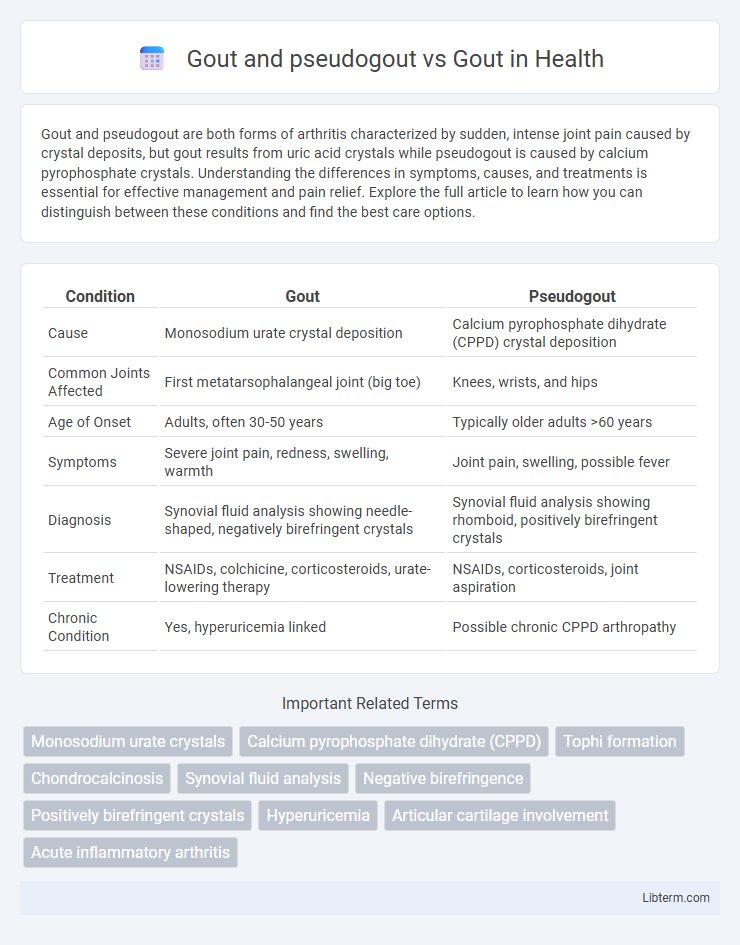
| Condition | Gout | Pseudogout |
|---|---|---|
| Cause | Monosodium urate crystal deposition | Calcium pyrophosphate dihydrate (CPPD) crystal deposition |
| Common Joints Affected | First metatarsophalangeal joint (big toe) | Knees, wrists, and hips |
| Age of Onset | Adults, often 30-50 years | Typically older adults >60 years |
| Symptoms | Severe joint pain, redness, swelling, warmth | Joint pain, swelling, possible fever |
| Diagnosis | Synovial fluid analysis showing needle-shaped, negatively birefringent crystals | Synovial fluid analysis showing rhomboid, positively birefringent crystals |
| Treatment | NSAIDs, colchicine, corticosteroids, urate-lowering therapy | NSAIDs, corticosteroids, joint aspiration |
| Chronic Condition | Yes, hyperuricemia linked | Possible chronic CPPD arthropathy |
Introduction to Gout and Pseudogout
Gout and pseudogout are types of inflammatory arthritis caused by crystal deposition in the joints, with gout resulting from monosodium urate crystals and pseudogout from calcium pyrophosphate dihydrate crystals. Both conditions lead to acute joint inflammation, but gout commonly affects the first metatarsophalangeal joint, whereas pseudogout frequently involves larger joints like the knees. Accurate differentiation using joint aspiration and crystal analysis is essential for effective treatment and management.
Defining Gout: Causes and Risk Factors
Gout is a form of inflammatory arthritis characterized by the accumulation of monosodium urate crystals in joints, primarily caused by hyperuricemia, or elevated uric acid levels in the blood. Risk factors for gout include obesity, high purine diet, excessive alcohol consumption, hypertension, and certain genetic predispositions. Unlike pseudogout, which involves calcium pyrophosphate crystal deposition, gout's pathogenesis centers on urate crystal formation leading to acute and chronic joint inflammation.
Understanding Pseudogout: Etiology and Triggers
Pseudogout, also known as calcium pyrophosphate deposition disease (CPPD), is caused by the accumulation of calcium pyrophosphate crystals in the joints, contrasting with gout, which results from monosodium urate crystal deposition. The etiology of pseudogout includes factors such as aging, joint trauma, metabolic disorders like hyperparathyroidism, and genetic predisposition. Triggers for pseudogout flare-ups often involve stress on the joints, surgery, or illnesses, whereas gout flares are typically induced by hyperuricemia and dietary factors.
Gout vs. Pseudogout: Key Differences
Gout is caused by the deposition of monosodium urate crystals due to hyperuricemia, while pseudogout results from calcium pyrophosphate dihydrate crystal accumulation. Clinically, gout typically presents with sudden, severe joint pain mainly affecting the first metatarsophalangeal joint, whereas pseudogout commonly involves larger joints like the knee and unfolds more gradually. Diagnostic differentiation relies on joint fluid analysis revealing needle-shaped, negatively birefringent crystals in gout and rhomboid-shaped, positively birefringent crystals in pseudogout.
Clinical Presentation: Symptoms Comparison
Gout typically presents with sudden, intense joint pain, redness, swelling, and warmth, often affecting the first metatarsophalangeal joint (big toe). Pseudogout symptoms resemble gout but usually involve larger joints like the knees or wrists, with less intense pain and a more gradual onset. Both conditions cause joint inflammation, but gout flares are more abruptly painful and recurrent, while pseudogout episodes last longer with milder inflammation.
Diagnostic Approaches: Gout and Pseudogout
Synovial fluid analysis remains the gold standard for differentiating gout and pseudogout, where monosodium urate crystals indicate gout, and calcium pyrophosphate dihydrate crystals confirm pseudogout. Advanced imaging techniques like dual-energy CT scans enhance gout diagnosis by detecting urate crystal deposits, whereas chondrocalcinosis on X-rays suggests pseudogout. Accurate diagnosis relies on crystal identification combined with clinical presentation and serum uric acid levels.
Crystal Identification: Uric Acid vs. Calcium Pyrophosphate
Gout is characterized by the deposition of monosodium urate crystals, identifiable under polarized light microscopy as needle-shaped and negatively birefringent. Pseudogout involves calcium pyrophosphate crystals, which appear rhomboid-shaped and positively birefringent. Accurate crystal identification through joint fluid analysis remains the diagnostic gold standard to differentiate between uric acid and calcium pyrophosphate deposition diseases.
Treatment Strategies: Gout vs. Pseudogout
Treatment strategies for gout primarily involve urate-lowering therapy such as allopurinol or febuxostat to reduce serum uric acid levels, alongside NSAIDs, colchicine, or corticosteroids for acute flare management. Pseudogout treatment focuses on controlling inflammation using NSAIDs, colchicine, and corticosteroids without urate-lowering agents, as calcium pyrophosphate dihydrate crystal deposition is the underlying cause. Long-term management of pseudogout emphasizes addressing joint damage and minimizing flare frequency rather than reducing serum uric acid.
Complications and Prognosis
Gout complications include chronic arthritis, tophi formation, joint destruction, and increased risk of cardiovascular disease, with a generally favorable prognosis if appropriately managed through urate-lowering therapy and lifestyle modifications. Pseudogout complications primarily involve recurrent joint inflammation and cartilage damage, potentially leading to chronic arthritis, but it lacks the systemic cardiovascular risks seen in gout; prognosis depends on controlling calcium pyrophosphate crystal deposition and managing acute attacks. Both conditions require early diagnosis and treatment to prevent long-term joint damage and improve patient outcomes.
Prevention and Lifestyle Modifications
Effective prevention of gout and pseudogout focuses on managing risk factors through lifestyle modifications such as maintaining a healthy weight, staying hydrated, and limiting intake of purine-rich foods like red meat and seafood. Regular exercise and avoiding excessive alcohol consumption, especially beer and spirits, help reduce flare-ups by lowering uric acid levels in gout and calcium pyrophosphate crystal formation in pseudogout. Incorporating a balanced diet rich in low-fat dairy, vitamin C, and whole grains supports joint health and minimizes the frequency of acute attacks in both conditions.
Gout and pseudogout Infographic
 libterm.com
libterm.com