Monocytosis is a condition characterized by an elevated number of monocytes in the bloodstream, often signaling chronic inflammation or infections such as tuberculosis and certain autoimmune disorders. Monitoring your monocyte levels can provide crucial insights into your immune system's response and help in diagnosing underlying health issues. Explore more about the causes, symptoms, and treatments of monocytosis in the full article.
Table of Comparison
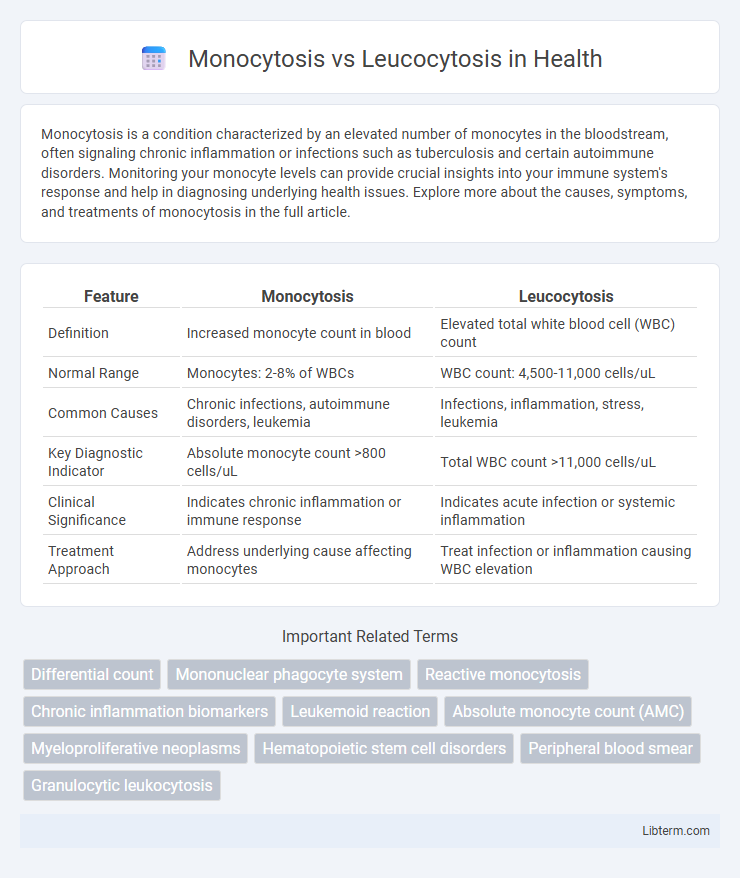
| Feature | Monocytosis | Leucocytosis |
|---|---|---|
| Definition | Increased monocyte count in blood | Elevated total white blood cell (WBC) count |
| Normal Range | Monocytes: 2-8% of WBCs | WBC count: 4,500-11,000 cells/uL |
| Common Causes | Chronic infections, autoimmune disorders, leukemia | Infections, inflammation, stress, leukemia |
| Key Diagnostic Indicator | Absolute monocyte count >800 cells/uL | Total WBC count >11,000 cells/uL |
| Clinical Significance | Indicates chronic inflammation or immune response | Indicates acute infection or systemic inflammation |
| Treatment Approach | Address underlying cause affecting monocytes | Treat infection or inflammation causing WBC elevation |
Understanding Monocytosis and Leucocytosis
Monocytosis is characterized by an elevated monocyte count in the blood, often signaling chronic infections, inflammation, or certain malignancies, while leucocytosis refers to a broader increase in total white blood cells, indicating acute infections, stress, or bone marrow disorders. Differentiating monocytosis from leucocytosis involves analyzing specific white cell subsets to target underlying causes accurately. Accurate diagnosis requires correlating clinical symptoms with complete blood count results and differential white cell counts to guide appropriate treatment.
Definition and Key Differences
Monocytosis is defined as an increased number of monocytes in the blood, typically exceeding 1,000 cells per microliter, often indicative of chronic inflammation or infection. Leucocytosis refers to an elevated total white blood cell count, generally above 11,000 cells per microliter, encompassing increases in various leukocyte types including neutrophils, lymphocytes, and monocytes. The key difference lies in monocytosis being a subtype of leucocytosis specifically involving monocytes, whereas leucocytosis represents a broader increase in multiple white blood cell types.
Causes of Monocytosis
Monocytosis is primarily caused by chronic infections such as tuberculosis, certain autoimmune diseases like lupus, and hematologic disorders including chronic myelomonocytic leukemia. In contrast, leucocytosis encompasses a broader range of causes, often triggered by acute infections, inflammation, stress, or bone marrow stimulation. Elevated monocyte counts specifically indicate prolonged immune response or tissue repair processes, distinguishing monocytosis from generalized leukocyte elevation in leucocytosis.
Causes of Leucocytosis
Leucocytosis is primarily caused by infections, inflammation, stress, trauma, or hematologic disorders such as leukemia, whereas monocytosis specifically indicates increased monocyte counts often linked to chronic infections, autoimmune diseases, or certain malignancies. Infections like bacterial pneumonia or tuberculosis can elevate overall white blood cell counts, contributing to leucocytosis. Certain medications, smoking, and recovery from neutropenia also induce leucocytosis by stimulating white blood cell production.
Clinical Significance and Implications
Monocytosis indicates an elevated monocyte count often associated with chronic infections, autoimmune disorders, and hematologic malignancies, highlighting its role in ongoing immune response and inflammation. Leukocytosis refers to an increased total white blood cell count, commonly seen in acute infections, inflammation, stress, and leukemias, reflecting a general immune activation. Differentiating monocytosis from leukocytosis in clinical practice aids in diagnosing specific pathological conditions and tailoring targeted therapeutic interventions.
Diagnostic Criteria for Both Conditions
Monocytosis is characterized by an absolute monocyte count exceeding 1,000 cells/uL, often identified through a complete blood count (CBC) with differential showing increased monocytes above the normal range of 2-8%. Leucocytosis is defined by a total white blood cell count above the upper reference limit, typically greater than 11,000 cells/uL, indicating an overall increase in leukocytes including neutrophils, lymphocytes, monocytes, eosinophils, or basophils. Diagnostic criteria rely on CBC results, with monocytosis specifying monocyte elevation while leucocytosis refers to a generalized leukocyte increase, which helps differentiate underlying causes such as infections, inflammation, or hematologic disorders.
Common Symptoms and Manifestations
Monocytosis is characterized by an elevated monocyte count in the blood, commonly presenting with symptoms like fever, fatigue, night sweats, and weight loss, often indicating chronic infections or inflammatory conditions. Leucocytosis involves a general increase in white blood cells, with manifestations such as fever, chills, and signs of infection or inflammation, reflecting an acute or systemic response. Both conditions may share symptoms like malaise and swelling but differ mainly in the specific white cell subtype elevated and associated underlying causes.
Laboratory Evaluation and Interpretation
Monocytosis is characterized by an elevated monocyte count, typically above 800 cells/uL, often indicating chronic infections, autoimmune disorders, or hematologic malignancies, with laboratory evaluation relying on complete blood count (CBC) and peripheral smear analysis to identify abnormal monocyte morphology. Leucocytosis refers to an increased total white blood cell count, usually above 11,000 cells/uL, commonly associated with acute infections, inflammation, stress, or myeloproliferative disorders, and is assessed by differential WBC count to determine the specific leukocyte subtypes involved. Interpreting these results requires correlating clinical context with CBC findings, including absolute monocyte count for monocytosis and total leukocyte count plus differential percentages for leucocytosis to guide further diagnostic and therapeutic steps.
Treatment Approaches and Management
Monocytosis treatment targets underlying causes such as infections, chronic inflammation, or hematologic disorders, often involving antimicrobial therapy, corticosteroids, or chemotherapy for malignancies. Leucocytosis management depends on the specific etiology, with infection-driven cases typically treated using antibiotics, while reactive or stress-induced leucocytosis might require supportive care and monitoring. Both conditions necessitate regular blood count assessments and addressing primary diseases to normalize white blood cell levels effectively.
Prognosis and Patient Outcomes
Monocytosis indicates an elevated monocyte count often linked to chronic infections, autoimmune diseases, or malignancies, with prognosis varying based on the underlying condition's severity and response to treatment. Leukocytosis reflects a broad increase in white blood cells and may signify acute infections, inflammation, or hematologic disorders, where patient outcomes depend on timely diagnosis and effective management of the causative disease. Both conditions require targeted interventions to improve prognosis, with monocytosis sometimes predicting chronic or progressive illness, while leukocytosis often resolves with treatment of the primary cause.
Monocytosis Infographic
 libterm.com
libterm.com