Recurrence occurs when a disease or condition returns after a period of improvement or remission, often signaling the need for further treatment or monitoring. Understanding the factors that contribute to recurrence can help you take proactive steps to prevent its reappearance and manage your health effectively. Explore the rest of the article to learn more about recurrence, its causes, and strategies to reduce your risk.
Table of Comparison
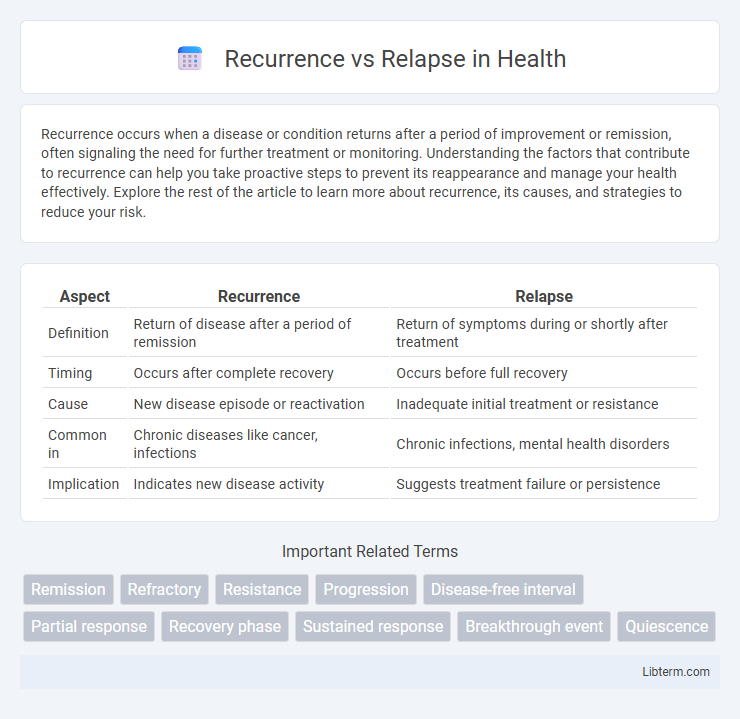
| Aspect | Recurrence | Relapse |
|---|---|---|
| Definition | Return of disease after a period of remission | Return of symptoms during or shortly after treatment |
| Timing | Occurs after complete recovery | Occurs before full recovery |
| Cause | New disease episode or reactivation | Inadequate initial treatment or resistance |
| Common in | Chronic diseases like cancer, infections | Chronic infections, mental health disorders |
| Implication | Indicates new disease activity | Suggests treatment failure or persistence |
Introduction to Recurrence and Relapse
Recurrence refers to the return of disease symptoms after a period of improvement, often indicating the same condition re-emerging following treatment success. Relapse specifically describes the reappearance of cancer or chronic disease symptoms during or shortly after completing therapy, reflecting an incomplete eradication of the illness. Understanding the distinction between recurrence and relapse is crucial for tailoring patient management and optimizing long-term outcomes.
Defining Recurrence: What Does It Mean?
Recurrence refers to the return of a disease or its symptoms after a period of improvement or remission, indicating the disease has re-emerged following treatment. It implies that the underlying condition was not fully eradicated and reactivates after a symptom-free interval. Medical professionals distinguish recurrence from relapse based on timing and disease activity, with recurrence often signifying a new phase of the disease process.
Understanding Relapse: A Comprehensive Overview
Relapse refers to the return of symptoms or disease after a period of improvement or remission, often indicating the resurgence of the same condition. It is crucial to distinguish relapse from recurrence, as relapse typically implies the original illness was suppressed but not eradicated, whereas recurrence may indicate a new episode. Understanding relapse involves recognizing triggers, monitoring early signs, and implementing timely interventions to prevent full disease reactivation.
Key Differences Between Recurrence and Relapse
Recurrence refers to the return of a medical condition or symptoms after a period of improvement or remission, often due to the original disease reactivating or reemerging. Relapse specifically denotes the worsening or return of symptoms in a previously treated condition, typically within a short timeframe after apparent recovery. Key differences include timing and cause: recurrence may occur after a longer symptom-free interval, while relapse usually happens quickly due to incomplete treatment or unresolved underlying issues.
Common Causes of Recurrence and Relapse
Recurrence and relapse often stem from factors such as incomplete treatment, persistent risk behaviors, and underlying health conditions worsening over time. Common causes include failure to adhere to medication regimens, exposure to triggering environments, and untreated co-morbidities like mental health disorders or substance abuse. Identifying these causes is crucial for developing targeted prevention strategies and improving long-term patient outcomes.
Risk Factors and Predictors
Recurrence in medical conditions refers to the return of disease symptoms or pathology after a period of remission, often influenced by risk factors such as genetic predisposition, unresolved underlying causes, and lifestyle behaviors. Relapse specifically denotes the return of symptoms in chronic diseases like psychiatric disorders or cancer, with predictors including treatment non-adherence, environmental stressors, and biomarker fluctuations. Identifying risk factors like inflammation markers, family history, and early symptom patterns significantly improves prediction models for both recurrence and relapse, enabling targeted prevention strategies.
Clinical Implications for Treatment
Recurrence and relapse differ in clinical implications, as recurrence refers to the return of a disease after a period of remission, often necessitating a re-evaluation of treatment protocols and possibly more aggressive therapy. Relapse indicates the worsening of symptoms during ongoing treatment, signaling potential resistance to current medications and the need for alternative therapeutic strategies. Understanding these distinctions informs personalized treatment plans and improves patient outcomes in chronic conditions like cancer and mental health disorders.
Prevention Strategies for Both Recurrence and Relapse
Effective prevention strategies for recurrence and relapse involve consistent adherence to treatment plans and ongoing monitoring of symptoms. Engaging in regular therapy sessions, maintaining medication compliance, and adopting lifestyle modifications such as stress management and healthy routines significantly reduce risks. Early intervention upon warning signs and continuous support systems play a crucial role in sustaining long-term remission and preventing both recurrence and relapse.
Monitoring and Early Detection Methods
Monitoring and early detection methods for recurrence and relapse include regular imaging techniques such as CT scans, MRI, and PET scans, alongside biomarker analysis and liquid biopsies to identify minimal residual disease. Continuous surveillance through clinical exams, blood tests measuring tumor markers, and molecular diagnostic tools enhances timely identification of cancer return or progression. Implementing tailored follow-up protocols based on cancer type and risk factors significantly improves the chances of detecting recurrence versus relapse at an early, more treatable stage.
Conclusion: Managing Recurrence and Relapse Effectively
Managing recurrence and relapse effectively requires early detection and tailored treatment strategies based on the underlying cause and patient history. Continuous monitoring through clinical assessments and biomarker evaluations plays a critical role in preventing disease progression. Implementing personalized interventions and adhering to evidence-based guidelines improve long-term patient outcomes and reduce the risk of further episodes.
Recurrence Infographic
 libterm.com
libterm.com