Identifying risk factors is essential for understanding potential threats to your health, safety, or financial well-being. These elements can range from lifestyle choices and environmental influences to genetic predispositions, each contributing differently to the likelihood of adverse outcomes. Explore the rest of the article to learn how recognizing and managing risk factors can empower you to make informed decisions.
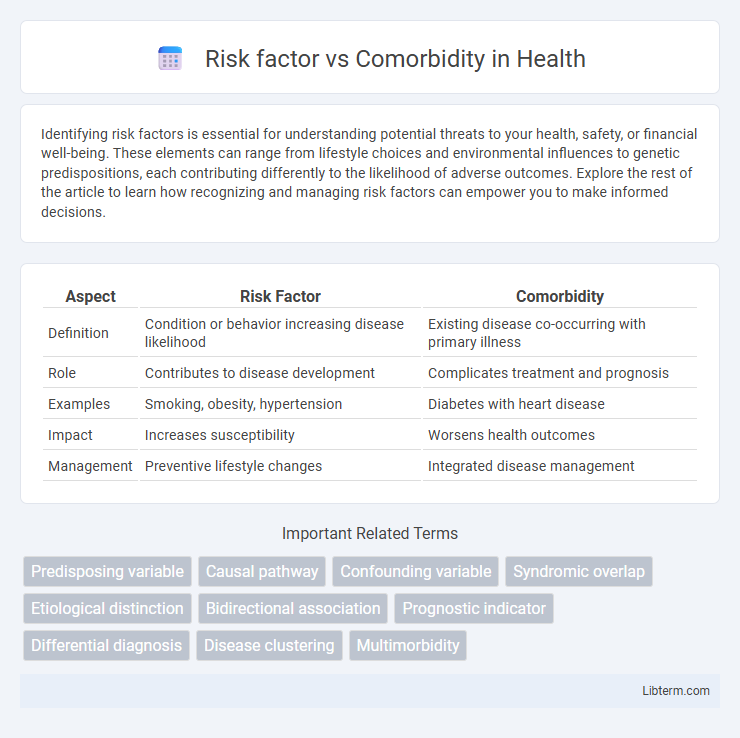
Table of Comparison
| Aspect | Risk Factor | Comorbidity |
|---|---|---|
| Definition | Condition or behavior increasing disease likelihood | Existing disease co-occurring with primary illness |
| Role | Contributes to disease development | Complicates treatment and prognosis |
| Examples | Smoking, obesity, hypertension | Diabetes with heart disease |
| Impact | Increases susceptibility | Worsens health outcomes |
| Management | Preventive lifestyle changes | Integrated disease management |
Understanding Risk Factors: Definitions and Types
Risk factors are characteristics or exposures that increase the likelihood of developing a disease, such as smoking for lung cancer or high blood pressure for heart disease. Comorbidities refer to the presence of one or more additional medical conditions co-occurring with a primary condition, often complicating treatment and prognosis. Understanding risk factors involves identifying modifiable (e.g., lifestyle behaviors) and non-modifiable elements (e.g., genetics or age) that contribute to disease susceptibility and prevention strategies.
What Are Comorbidities? An Overview
Comorbidities refer to the presence of one or more additional medical conditions co-occurring with a primary disease, significantly affecting diagnosis, treatment, and prognosis. Unlike risk factors that increase the likelihood of developing a disease, comorbidities represent pre-existing or concurrent illnesses, such as diabetes or hypertension, that complicate patient management. Understanding comorbidities is crucial for comprehensive healthcare planning and optimizing patient outcomes in chronic and acute conditions.
Key Differences Between Risk Factors and Comorbidities
Risk factors are variables or behaviors that increase the likelihood of developing a disease, such as smoking for lung cancer, while comorbidities are existing additional medical conditions that coexist with a primary disease, often complicating treatment outcomes. Risk factors contribute to disease onset, whereas comorbidities influence disease progression and management. Understanding the distinction between risk factors and comorbidities is crucial for effective diagnosis, prevention, and personalized treatment planning.
Identifying Risk Factors in Disease Development
Risk factors are specific characteristics or exposures that increase the likelihood of developing a disease, such as smoking for lung cancer or high blood pressure for cardiovascular disease. Comorbidities refer to the simultaneous presence of two or more chronic diseases or conditions in a patient, which can complicate treatment and prognosis. Identifying risk factors in disease development involves analyzing patient history, environmental exposure, genetic predispositions, and lifestyle choices to implement early intervention and preventive healthcare strategies.
The Role of Comorbidities in Patient Outcomes
Comorbidities significantly affect patient outcomes by increasing the complexity of disease management and elevating the risk of complications during treatment. Unlike risk factors that predict the likelihood of developing a condition, comorbidities represent existing chronic diseases that interact with the primary illness, often worsening prognosis and increasing mortality rates. Understanding the role of comorbidities enables healthcare providers to tailor treatment plans and improve overall patient care efficiency.
How Risk Factors Contribute to Comorbid Conditions
Risk factors such as smoking, obesity, and hypertension significantly increase the likelihood of developing comorbid conditions like diabetes, cardiovascular disease, and chronic respiratory disorders. These risk factors trigger physiological changes that exacerbate existing health issues, leading to a complex interplay between multiple illnesses. Understanding how modifiable risk factors contribute to comorbidities enables targeted prevention strategies and improved clinical outcomes.
Clinical Implications: Managing Risk Factors vs. Comorbidities
Effective management of risk factors like hypertension and obesity involves preventive strategies to reduce disease onset, whereas addressing comorbidities such as diabetes alongside cardiovascular disease requires integrated treatment plans to improve patient outcomes. Clinical approaches prioritize early identification and modification of risk factors to prevent disease progression, while comorbidity management focuses on coordinated care to mitigate compounded health risks and complications. Tailoring interventions based on whether a condition is a risk factor or comorbidity enhances therapeutic efficacy and optimizes healthcare resource utilization.
Assessing Patient History: Screening for Risk vs. Comorbidity
Assessing patient history requires distinguishing between risk factors, such as smoking or obesity, which increase the likelihood of developing a disease, and comorbidities like diabetes or hypertension, which are existing co-occurring conditions. Screening for risk factors involves identifying behaviors and exposures that predispose patients to future health issues, while screening for comorbidities focuses on detecting chronic illnesses that may complicate treatment outcomes. Accurate differentiation improves clinical decision-making and personalized care planning by addressing both prevention and management strategies.
Prevention Strategies: Reducing Risk Factors
Reducing risk factors such as smoking, poor diet, and physical inactivity is essential in preventing the development of chronic diseases before comorbidities arise. Targeted prevention strategies like health education, lifestyle modifications, and regular screenings can effectively lower the incidence of risk factors that lead to conditions such as hypertension and diabetes. Addressing these modifiable risk factors early reduces the burden of multiple comorbidities and improves long-term health outcomes.
Treatment Considerations for Patients with Comorbidities
Treatment considerations for patients with comorbidities require careful evaluation of drug interactions, potential side effects, and disease progression risks. Tailoring therapeutic regimens involves prioritizing medications that minimize adverse effects while addressing multiple conditions simultaneously. Coordinated care among specialists enhances outcomes by integrating management strategies that target both the primary illness and coexisting health issues.
Risk factor Infographic
 libterm.com
libterm.com