Hemorrhage refers to the excessive or uncontrolled bleeding that can occur internally or externally due to injury, medical conditions, or vascular abnormalities. Prompt recognition and management are crucial to prevent severe complications or death. Explore the rest of this article to understand the causes, symptoms, and treatments that can help protect your health.
Table of Comparison
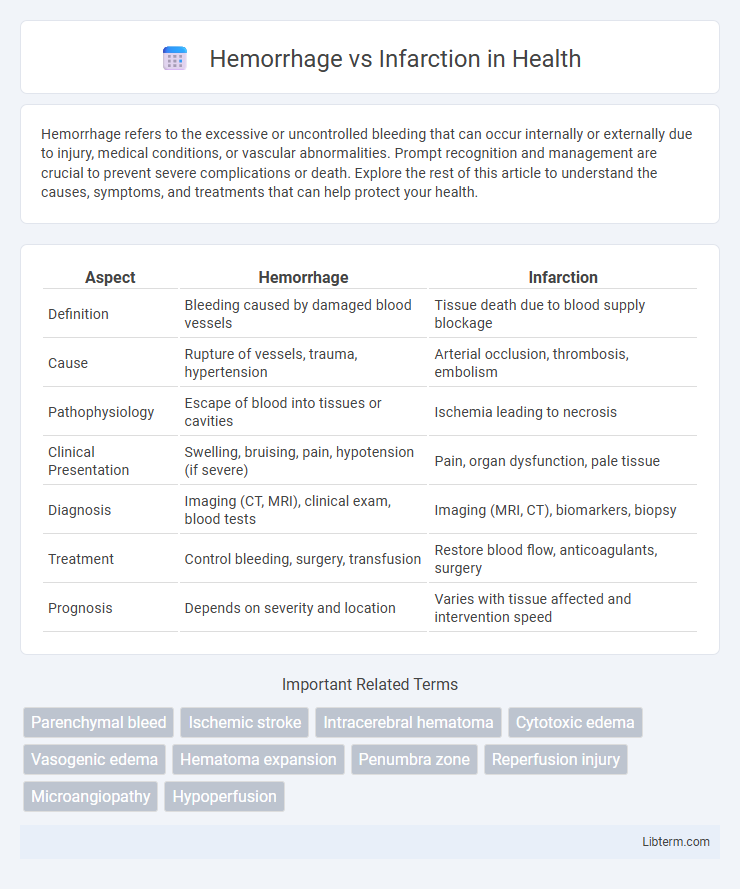
| Aspect | Hemorrhage | Infarction |
|---|---|---|
| Definition | Bleeding caused by damaged blood vessels | Tissue death due to blood supply blockage |
| Cause | Rupture of vessels, trauma, hypertension | Arterial occlusion, thrombosis, embolism |
| Pathophysiology | Escape of blood into tissues or cavities | Ischemia leading to necrosis |
| Clinical Presentation | Swelling, bruising, pain, hypotension (if severe) | Pain, organ dysfunction, pale tissue |
| Diagnosis | Imaging (CT, MRI), clinical exam, blood tests | Imaging (MRI, CT), biomarkers, biopsy |
| Treatment | Control bleeding, surgery, transfusion | Restore blood flow, anticoagulants, surgery |
| Prognosis | Depends on severity and location | Varies with tissue affected and intervention speed |
Introduction to Hemorrhage and Infarction
Hemorrhage refers to the escape of blood from ruptured blood vessels, leading to localized or widespread bleeding that disrupts normal tissue function. Infarction occurs when blood supply to an area is obstructed, causing tissue death due to ischemia and oxygen deprivation. Both conditions involve vascular injury but differ fundamentally in their mechanisms--hemorrhage results from vessel rupture, while infarction results from vessel occlusion.
Defining Hemorrhage: Causes and Types
Hemorrhage refers to the escape of blood from damaged blood vessels, caused by trauma, hypertension, aneurysm rupture, or coagulation disorders. There are various types of hemorrhages, including intracerebral, subarachnoid, subdural, and epidural hemorrhages, each distinguished by their location within or around the brain tissue. Understanding the causes and classification of hemorrhages is essential for accurate diagnosis and effective treatment.
Understanding Infarction: Causes and Variants
Infarction occurs due to the sudden obstruction of blood supply, leading to tissue ischemia and necrosis, with causes including arterial thrombosis, embolism, and vasospasm. Variants of infarction depend on tissue type and blood supply, such as red (hemorrhagic) infarcts in organs with dual blood supply like lungs, and pale (anemic) infarcts in solid organs like the heart and kidneys. Understanding the pathophysiology and vascular anatomy is crucial for differentiating infarction from hemorrhage and guiding clinical management.
Key Differences Between Hemorrhage and Infarction
Hemorrhage involves the escape of blood from ruptured vessels leading to tissue damage, while infarction results from the obstruction of blood supply causing tissue death due to ischemia. Hemorrhage is characterized by bleeding potentially causing increased intracranial pressure or hypovolemic shock, whereas infarction presents with localized necrosis primarily due to arterial or venous occlusion. Diagnostic differentiation relies on imaging modalities like CT or MRI, where hemorrhage appears as hyperdense areas indicative of bleeding, and infarction shows hypodense zones reflecting necrosis and edema.
Clinical Presentation: Symptoms and Signs
Hemorrhage typically presents with sudden onset of severe headache, nausea, vomiting, and focal neurological deficits such as weakness or altered consciousness, often accompanied by signs of increased intracranial pressure. Infarction usually manifests as gradual or sudden focal neurological deficits like unilateral weakness, aphasia, or sensory loss, with symptoms evolving over minutes to hours and often without headache. Both conditions may show altered mental status, but hemorrhage more frequently causes rapid deterioration due to mass effect and vascular disruption.
Diagnostic Approaches for Hemorrhage and Infarction
Diagnostic approaches for hemorrhage primarily involve imaging techniques such as non-contrast computed tomography (CT) scans, which quickly identify acute bleeding in the brain or other tissues. Magnetic resonance imaging (MRI) with susceptibility-weighted imaging (SWI) enhances detection of microbleeds and hemorrhagic transformations. In contrast, infarction diagnosis relies on diffusion-weighted MRI (DWI) to detect ischemic areas early, while CT perfusion imaging assesses cerebral blood flow deficits indicating infarcted tissue.
Imaging Findings: CT and MRI Comparison
Hemorrhage typically appears hyperdense on CT scans due to acute blood presence, often showing a well-defined high-attenuation area, whereas infarction initially presents as hypodense regions indicating ischemic tissue loss. MRI offers greater specificity; hemorrhages demonstrate variable signal intensities on T1- and T2-weighted images depending on the age of the bleed, with susceptibility-weighted imaging (SWI) enhancing detection of blood products. Infarctions display restricted diffusion on diffusion-weighted imaging (DWI) sequences early on, with corresponding low apparent diffusion coefficient (ADC) values, distinguishing ischemic injury from hemorrhagic lesions.
Management Strategies for Hemorrhage
Management strategies for hemorrhage prioritize rapid hemostasis through surgical intervention or minimally invasive techniques such as embolization. Supportive care includes fluid resuscitation, blood transfusions, and correction of coagulopathies to stabilize hemodynamics. Close monitoring in intensive care units ensures early detection of complications, while pharmacologic agents like antifibrinolytics may reduce bleeding.
Treatment Modalities for Infarction
Treatment modalities for infarction primarily focus on restoring blood flow and minimizing tissue damage through interventions such as thrombolytic therapy, percutaneous coronary intervention (PCI), and anticoagulant administration. Early reperfusion techniques are critical in acute myocardial infarction to salvage ischemic myocardium and improve patient outcomes. Supportive care including oxygen therapy, pain management, and monitoring for complications also plays a crucial role in infarction management.
Prognosis and Outcomes: Hemorrhage vs Infarction
Hemorrhage often leads to increased intracranial pressure and can cause rapid neurological deterioration, with prognosis heavily influenced by the size, location, and management of bleeding. Infarction results from vascular occlusion causing ischemic tissue death, and its outcome depends on the extent of brain damage and the timing of reperfusion therapies. Overall, hemorrhagic events generally have higher immediate mortality, while infarctions may result in variable long-term disability based on stroke severity and rehabilitation success.
Hemorrhage Infographic
 libterm.com
libterm.com