Intracerebral hemorrhage occurs when a blood vessel within the brain bursts, leading to bleeding inside the brain tissue that can cause significant damage and affect neurological functions. Symptoms can include sudden headache, weakness, confusion, and loss of consciousness, requiring immediate medical attention to prevent severe complications. Discover detailed insights into causes, symptoms, treatment options, and recovery strategies in the rest of the article.
Table of Comparison
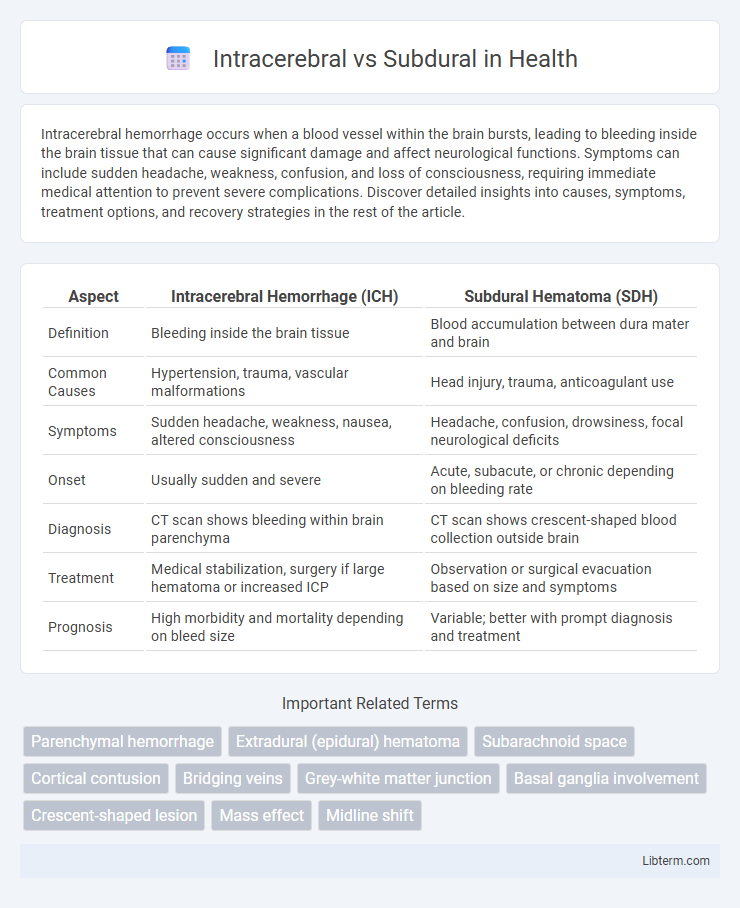
| Aspect | Intracerebral Hemorrhage (ICH) | Subdural Hematoma (SDH) |
|---|---|---|
| Definition | Bleeding inside the brain tissue | Blood accumulation between dura mater and brain |
| Common Causes | Hypertension, trauma, vascular malformations | Head injury, trauma, anticoagulant use |
| Symptoms | Sudden headache, weakness, nausea, altered consciousness | Headache, confusion, drowsiness, focal neurological deficits |
| Onset | Usually sudden and severe | Acute, subacute, or chronic depending on bleeding rate |
| Diagnosis | CT scan shows bleeding within brain parenchyma | CT scan shows crescent-shaped blood collection outside brain |
| Treatment | Medical stabilization, surgery if large hematoma or increased ICP | Observation or surgical evacuation based on size and symptoms |
| Prognosis | High morbidity and mortality depending on bleed size | Variable; better with prompt diagnosis and treatment |
Introduction to Brain Hemorrhages
Intracerebral hemorrhage occurs when a blood vessel bursts directly within the brain tissue, leading to localized bleeding that can cause increased intracranial pressure and neuronal damage. Subdural hemorrhage involves bleeding between the dura mater and the arachnoid membrane, often resulting from traumatic injury that tears bridging veins, producing a crescent-shaped hematoma on imaging. Both types of brain hemorrhages disrupt normal neural function and require urgent medical evaluation to prevent severe neurological deficits or death.
Defining Intracerebral Hemorrhage
Intracerebral hemorrhage (ICH) is a type of stroke characterized by bleeding directly into the brain tissue, often caused by hypertension, arteriovenous malformations, or trauma. Unlike subdural hematomas, which involve bleeding between the dura mater and the brain surface, ICH results in increased intracranial pressure and localized brain damage. Accurate diagnosis through CT or MRI is crucial for differentiating ICH from subdural hemorrhage and guiding effective treatment strategies.
Defining Subdural Hematoma
Subdural hematoma is a type of traumatic brain injury characterized by the accumulation of blood between the dura mater and the arachnoid membrane, often caused by vessel rupture due to head trauma. Intracerebral hematoma, in contrast, involves bleeding directly within the brain tissue itself, leading to localized pressure and potential brain damage. Distinguishing subdural hematomas from intracerebral hemorrhages is crucial for diagnosis and treatment, as subdural hematomas primarily involve venous bleeding while intracerebral hemorrhages usually result from arterial injury or hypertension.
Key Causes and Risk Factors
Intracerebral hemorrhage primarily results from hypertension-induced vessel rupture, cerebral amyloid angiopathy, or vascular malformations, with hypertension and advanced age as major risk factors. Subdural hematomas commonly stem from head trauma causing bridging vein tears, particularly in elderly patients, individuals on anticoagulant therapy, and those with brain atrophy. Both conditions share trauma as a critical cause but differ in vascular involvement and typical patient profiles.
Clinical Presentation and Symptoms
Intracerebral hemorrhage typically presents with sudden focal neurological deficits such as hemiparesis, aphasia, or altered consciousness due to bleeding within brain tissue. Subdural hematomas often manifest with progressive headache, confusion, and fluctuating levels of consciousness, reflecting blood accumulation between the dura and arachnoid layers. Both conditions may cause increased intracranial pressure symptoms, but subdural hematomas often have a more insidious onset compared to the acute presentation of intracerebral hemorrhage.
Diagnostic Approaches and Imaging
Intracerebral hemorrhages are best identified using non-contrast CT scans, which provide rapid visualization of bleeding within the brain parenchyma, while subdural hematomas appear as crescent-shaped hyperdensities along the brain surface on imaging. MRI and CT angiography further aid in differentiating the source and extent of hemorrhage, with MRI offering superior soft tissue contrast to assess associated brain injury or edema. Advanced imaging techniques like diffusion-weighted imaging and susceptibility-weighted imaging enhance diagnostic accuracy, guiding timely clinical management for both intracerebral and subdural hemorrhages.
Pathophysiological Differences
Intracerebral hemorrhage involves bleeding directly into the brain parenchyma caused by vessel rupture, leading to localized tissue destruction and increased intracranial pressure. Subdural hematoma results from venous bleeding between the dura mater and arachnoid membrane, typically from bridging vein rupture, causing a slower accumulation of blood and brain compression. The pathophysiology of intracerebral hemorrhage mainly centers on arterial bleeding and neurotoxicity from blood products, whereas subdural hematoma primarily involves venous bleeding and mechanical brain displacement.
Treatment and Management Strategies
Intracerebral hemorrhage treatment centers on stabilizing vital signs, managing intracranial pressure through medications like mannitol or hypertonic saline, and surgical intervention such as hematoma evacuation when necessary. Subdural hematoma management depends on the hematoma size and patient symptoms; small, asymptomatic subdural hematomas often require close monitoring with serial imaging, while larger or symptomatic cases typically necessitate surgical drainage via burr hole or craniotomy. Both conditions demand vigilant neurological assessment and prevention of secondary brain injury through optimized blood pressure control and supportive care in an intensive care setting.
Prognosis and Patient Outcomes
Intracerebral hemorrhage (ICH) typically presents a poorer prognosis compared to subdural hematoma (SDH) due to the direct damage to brain tissue and higher risk of increased intracranial pressure. Patient outcomes in ICH often involve higher mortality rates and long-term neurological deficits, whereas SDH, particularly acute subdural hematoma, may have variable outcomes depending on the rapidity of surgical intervention. Early diagnosis and treatment in SDH cases generally improve patient survival and functional recovery, while ICH prognosis depends heavily on hematoma size, location, and patient comorbidities.
Preventative Measures and Future Directions
Preventative measures for intracerebral hemorrhage primarily focus on controlling hypertension, managing anticoagulant use, and promoting healthy lifestyle choices to reduce stroke risk. Subdural hematoma prevention emphasizes fall prevention in elderly populations, helmet use during high-risk activities, and early treatment of coagulopathies. Future directions involve advanced neuroimaging techniques for early detection, development of targeted therapies to minimize brain damage, and integration of AI for personalized risk assessment and intervention strategies.
Intracerebral Infographic
 libterm.com
libterm.com