Myoclonus involves sudden, involuntary muscle jerks that can affect various parts of the body, often disrupting daily activities and sleep. Understanding the causes, types, and treatment options is essential for managing symptoms effectively. Explore the rest of this article to learn how to identify and address your myoclonus challenges.
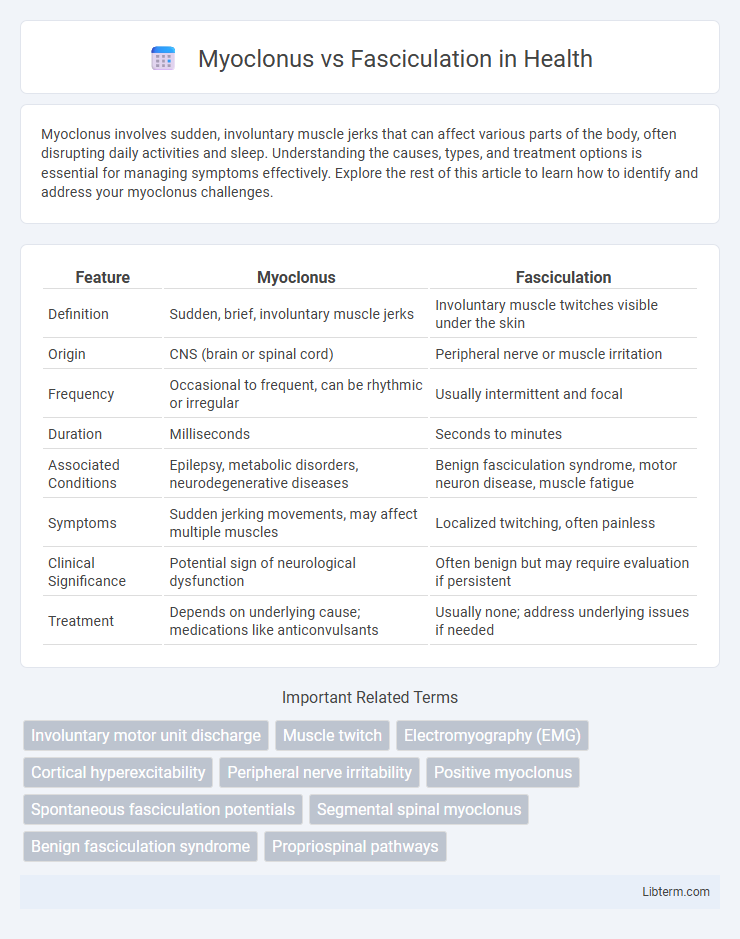
Table of Comparison
| Feature | Myoclonus | Fasciculation |
|---|---|---|
| Definition | Sudden, brief, involuntary muscle jerks | Involuntary muscle twitches visible under the skin |
| Origin | CNS (brain or spinal cord) | Peripheral nerve or muscle irritation |
| Frequency | Occasional to frequent, can be rhythmic or irregular | Usually intermittent and focal |
| Duration | Milliseconds | Seconds to minutes |
| Associated Conditions | Epilepsy, metabolic disorders, neurodegenerative diseases | Benign fasciculation syndrome, motor neuron disease, muscle fatigue |
| Symptoms | Sudden jerking movements, may affect multiple muscles | Localized twitching, often painless |
| Clinical Significance | Potential sign of neurological dysfunction | Often benign but may require evaluation if persistent |
| Treatment | Depends on underlying cause; medications like anticonvulsants | Usually none; address underlying issues if needed |
Introduction to Myoclonus and Fasciculation
Myoclonus refers to sudden, brief, involuntary muscle jerks caused by abnormal nerve activity in the brain or spinal cord, often linked to neurological disorders like epilepsy or metabolic imbalances. Fasciculations are spontaneous, fine muscle twitches resulting from the spontaneous firing of motor units, commonly seen in conditions such as amyotrophic lateral sclerosis (ALS) or benign fasciculation syndrome. Both phenomena involve muscle contractions but differ in their origin, appearance, and clinical significance, making accurate diagnosis crucial for effective management.
Definition of Myoclonus
Myoclonus is characterized by sudden, involuntary muscle jerks caused by rapid contractions or relaxations of muscles. Unlike fasciculations, which are small, involuntary muscle twitches visible under the skin, myoclonus involves larger, more forceful, and often rhythmic movements affecting various muscle groups. These jerks can result from neurological disorders, metabolic imbalances, or reactions to medications.
Definition of Fasciculation
Fasciculation refers to involuntary, spontaneous muscle fiber contractions visible as small twitches beneath the skin, often caused by nerve irritation or muscle fatigue. Unlike myoclonus, which involves sudden, brief muscle jerks, fasciculations are typically rhythmic and localized to small muscle groups. They are commonly observed in conditions like amyotrophic lateral sclerosis (ALS) but can also occur in benign scenarios.
Causes of Myoclonus
Myoclonus is caused by sudden, involuntary muscle jerks linked to neurological disorders such as epilepsy, metabolic imbalances, or brain injury, while fasciculations are minor, involuntary muscle twitches often related to benign causes like fatigue or anxiety. Myoclonus may also result from exposure to toxins, drug reactions, or infections affecting the central nervous system. Differentiating these conditions relies on understanding the underlying pathophysiology, with myoclonus involving hyperactive nerve signals in the brain or spinal cord.
Causes of Fasciculation
Fasciculations, characterized by involuntary muscle twitches, commonly result from benign causes such as muscle fatigue, stress, or caffeine intake. Pathological causes include motor neuron diseases like amyotrophic lateral sclerosis (ALS), peripheral neuropathies, electrolyte imbalances, and certain medications. Identifying the underlying etiology is critical for distinguishing fasciculations from myoclonus, which involves sudden, brief muscle jerks typically linked to neurological disorders like epilepsy or metabolic disturbances.
Clinical Presentation Differences
Myoclonus presents as sudden, brief, involuntary muscle jerks that can occur singly or in clusters, often involving larger muscle groups and affecting posture or movement. Fasciculations appear as small, involuntary muscle twitches beneath the skin, usually confined to a single muscle and not causing joint movement or functional impairment. Clinically, myoclonus is often associated with neurological disorders such as epilepsy or metabolic disturbances, whereas fasciculations are commonly linked to benign conditions like fatigue or more serious diseases like amyotrophic lateral sclerosis.
Diagnostic Approaches
Electromyography (EMG) is the primary diagnostic tool to distinguish myoclonus from fasciculations by analyzing muscle activity patterns; myoclonus presents as brief, sudden jerks with synchronous muscle firing, while fasciculations show irregular, spontaneous muscle fiber discharges. Clinical examination focuses on the distribution and triggers of involuntary movements, with myoclonus often involving larger, swift jerks, and fasciculations typically causing fine, localized twitches. Advanced neuroimaging and genetic testing may support diagnosis when underlying neurological disorders are suspected.
Associated Conditions and Syndromes
Myoclonus is commonly associated with neurological disorders such as epilepsy, Parkinson's disease, and Creutzfeldt-Jakob disease, often indicating cortical or subcortical dysfunction. Fasciculations are primarily linked to motor neuron diseases like amyotrophic lateral sclerosis (ALS) and benign fasciculation syndrome, with occasional presence in peripheral neuropathies. Understanding the distinct associated conditions helps differentiate these involuntary muscle movements and guides clinical diagnosis and management.
Treatment and Management Options
Myoclonus treatment primarily involves medications such as clonazepam, valproic acid, and levetiracetam to reduce sudden muscle jerks, while addressing underlying causes like metabolic disorders or neurodegenerative diseases is crucial for effective management. Fasciculation management often focuses on relieving symptoms and underlying causes, with options including magnesium supplements, addressing electrolyte imbalances, and treating conditions like benign fasciculation syndrome or motor neuron disease. Physical therapy and lifestyle modifications support both conditions by improving muscle function and reducing symptom severity.
Prognosis and Long-Term Outlook
Myoclonus often indicates underlying neurological disorders and its prognosis varies widely depending on the cause, with some forms being benign and others progressive or life-threatening. Fasciculations usually have a benign prognosis, especially when not accompanied by other neurological symptoms, but persistent fasciculations may warrant investigation for motor neuron diseases with a more guarded long-term outlook. Long-term management of myoclonus focuses on treating the root cause and symptom control, while fasciculations typically require monitoring for potential progression in rare cases.
Myoclonus Infographic
 libterm.com
libterm.com