Herpes Simplex Infection is a common viral condition caused by herpes simplex virus types 1 and 2, leading to painful blisters and sores primarily around the mouth or genital area. Understanding its transmission, symptoms, and treatment options is essential for managing outbreaks and reducing the risk of spread. Explore the rest of this article to learn how you can effectively recognize and control this infection.
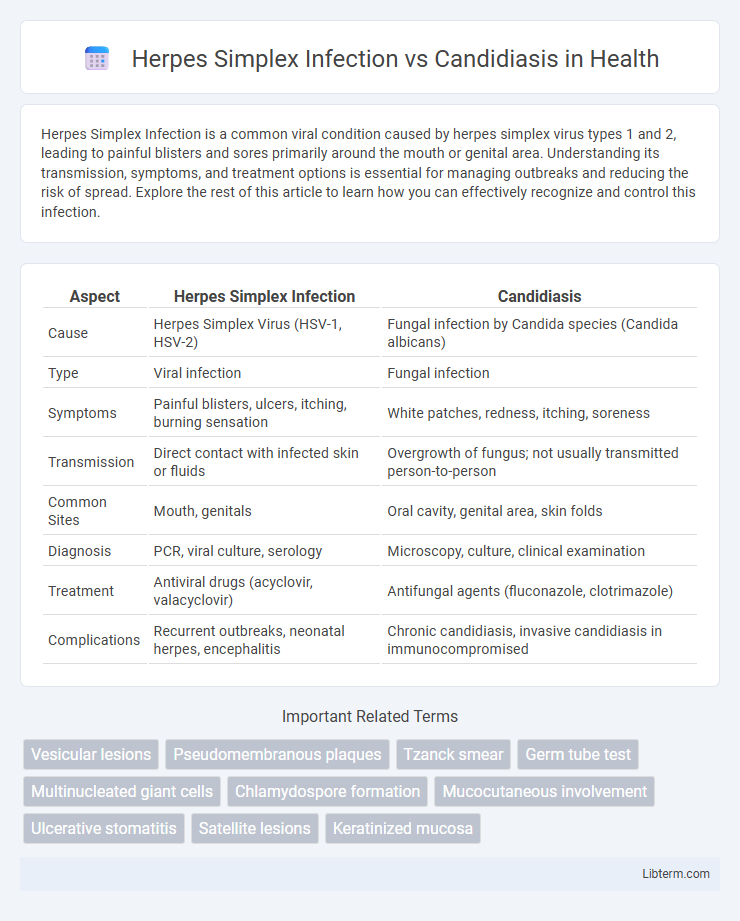
Table of Comparison
| Aspect | Herpes Simplex Infection | Candidiasis |
|---|---|---|
| Cause | Herpes Simplex Virus (HSV-1, HSV-2) | Fungal infection by Candida species (Candida albicans) |
| Type | Viral infection | Fungal infection |
| Symptoms | Painful blisters, ulcers, itching, burning sensation | White patches, redness, itching, soreness |
| Transmission | Direct contact with infected skin or fluids | Overgrowth of fungus; not usually transmitted person-to-person |
| Common Sites | Mouth, genitals | Oral cavity, genital area, skin folds |
| Diagnosis | PCR, viral culture, serology | Microscopy, culture, clinical examination |
| Treatment | Antiviral drugs (acyclovir, valacyclovir) | Antifungal agents (fluconazole, clotrimazole) |
| Complications | Recurrent outbreaks, neonatal herpes, encephalitis | Chronic candidiasis, invasive candidiasis in immunocompromised |
Overview of Herpes Simplex Infection and Candidiasis
Herpes Simplex Infection is a viral condition caused by the herpes simplex virus (HSV), presenting with painful, fluid-filled blisters primarily around the mouth or genital areas. Candidiasis is a fungal infection caused by Candida species, most commonly Candida albicans, manifesting as white patches and inflammation in moist areas like the mouth, throat, or genital region. Both infections affect mucosal surfaces but differ significantly in etiology, symptoms, and treatment approaches.
Etiological Agents: Virus vs Fungus
Herpes simplex infection is caused by the herpes simplex virus (HSV), primarily HSV-1 and HSV-2, which are DNA viruses belonging to the Herpesviridae family, responsible for mucocutaneous lesions and latent infections. In contrast, candidiasis is a fungal infection caused by Candida species, most commonly Candida albicans, a yeast-like fungus that can induce superficial and systemic infections by overgrowing on mucosal and cutaneous surfaces. The distinct etiological agents--a virus for herpes simplex and a fungus for candidiasis--result in differing pathogenesis, diagnostic approaches, and treatment strategies.
Modes of Transmission
Herpes Simplex Infection primarily spreads through direct contact with infected body fluids or skin lesions, typically via oral or genital routes during kissing, sexual activity, or childbirth. Candidiasis, caused by Candida species, transmits mainly through overgrowth of the yeast already present on mucosal surfaces or via indirect contact with contaminated objects in immunocompromised individuals. Understanding these distinct modes of transmission is crucial for effective prevention and control of both infections.
Common Clinical Manifestations
Herpes simplex infection commonly presents with painful, grouped vesicular lesions on erythematous bases, often accompanied by burning or tingling sensations before the outbreak. Candidiasis typically manifests as white, curd-like plaques on mucosal surfaces that can be wiped away, revealing erythematous, sometimes bleeding, underlying tissue. Both conditions may cause discomfort and inflammation, but herpes lesions are usually vesicular and ulcerative, whereas candidiasis is characterized by fungal overgrowth with distinct pseudomembranous plaques.
Key Differences in Symptoms
Herpes Simplex Infection typically presents with painful, grouped vesicular lesions on erythematous bases, often accompanied by fever, malaise, and lymphadenopathy. In contrast, Candidiasis manifests as white, curd-like plaques on mucous membranes, causing itching, burning, and redness without vesicular lesions. Herpes lesions often recur in the same location, while Candidiasis usually occurs in immunocompromised or diabetic patients and resolves with antifungal treatment.
Diagnostic Approaches and Laboratory Tests
Herpes Simplex Infection diagnosis primarily relies on PCR testing of lesion swabs to detect viral DNA, offering high sensitivity and specificity, while viral culture and direct fluorescent antibody tests provide supplementary confirmation. Candidiasis diagnosis involves microscopic examination and culture of clinical specimens such as oral swabs or vaginal discharge, with germ tube tests and chromogenic media aiding in species identification. Both infections may require serological assays in complex cases, but molecular methods remain the gold standard for HSV, whereas fungal culture remains essential for confirming candidiasis.
Treatment Strategies: Antivirals vs Antifungals
Herpes Simplex Infection treatment primarily involves antiviral medications such as acyclovir, valacyclovir, and famciclovir, which inhibit viral DNA replication and reduce symptom duration and frequency. In contrast, Candidiasis requires antifungal agents like fluconazole, clotrimazole, and amphotericin B that target fungal cell membranes and ergosterol biosynthesis to eradicate Candida species. Selecting the appropriate therapy depends on accurate diagnosis, with antivirals ineffective against fungal pathogens and antifungals incapable of controlling viral replication.
Risk Factors and Predisposing Conditions
Herpes Simplex Infection primarily affects individuals with weakened immune systems, such as those with HIV/AIDS, recipients of immunosuppressive therapy, or patients experiencing physical or emotional stress, increasing susceptibility to viral reactivation. In contrast, Candidiasis commonly occurs in people with diabetes mellitus, prolonged antibiotic use, or conditions causing mucosal barrier disruption, fostering Candida overgrowth. Both infections are influenced by factors like mucosal integrity, but viral latency in Herpes Simplex distinguishes its risk profile from the fungal colonization dynamics of Candidiasis.
Prevention and Infection Control
Herpes Simplex Infection prevention relies on consistent use of barrier methods such as condoms, along with avoiding direct contact with active lesions to reduce viral transmission. Infection control for Candidiasis emphasizes maintaining proper hygiene, controlling moisture in skin folds, and managing underlying risk factors like diabetes or immunosuppression to prevent fungal overgrowth. Regular screening and prompt treatment are critical in both infections to limit spread and recurrence.
Prognosis and Complications
Herpes Simplex Infection (HSV) prognosis is generally favorable, with recurrent episodes managed by antiviral therapy, while serious complications like encephalitis or neonatal herpes can occur in immunocompromised patients. Candidiasis prognosis depends on the infection site and host immunity, with mucocutaneous infections typically resolving after antifungal treatment, but invasive candidiasis can lead to life-threatening complications such as sepsis. Both infections require prompt diagnosis to prevent worsening outcomes, especially in individuals with compromised immune systems.
Herpes Simplex Infection Infographic
 libterm.com
libterm.com