Sialorrhea, characterized by excessive saliva production, often coexists with Gastroesophageal Reflux Disease (GERD), where acid reflux irritates the esophagus and triggers increased salivation as a protective response. Understanding the link between sialorrhea and GERD helps in identifying symptoms and tailoring effective treatment options to alleviate discomfort and improve your quality of life. Explore the rest of the article to learn more about these conditions and how to manage them effectively.
Table of Comparison
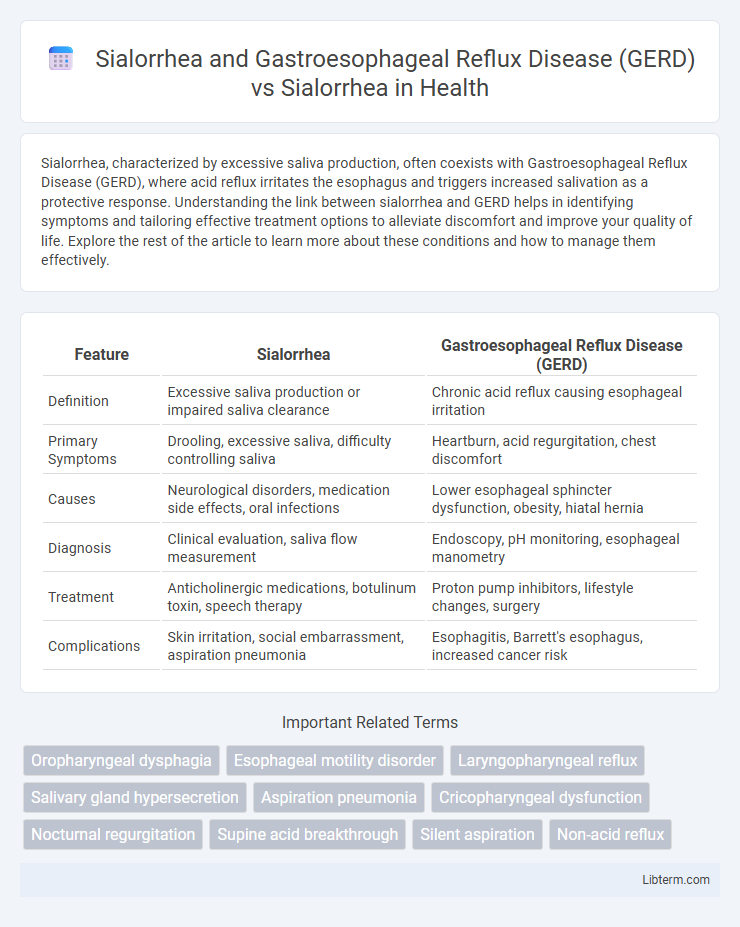
| Feature | Sialorrhea | Gastroesophageal Reflux Disease (GERD) |
|---|---|---|
| Definition | Excessive saliva production or impaired saliva clearance | Chronic acid reflux causing esophageal irritation |
| Primary Symptoms | Drooling, excessive saliva, difficulty controlling saliva | Heartburn, acid regurgitation, chest discomfort |
| Causes | Neurological disorders, medication side effects, oral infections | Lower esophageal sphincter dysfunction, obesity, hiatal hernia |
| Diagnosis | Clinical evaluation, saliva flow measurement | Endoscopy, pH monitoring, esophageal manometry |
| Treatment | Anticholinergic medications, botulinum toxin, speech therapy | Proton pump inhibitors, lifestyle changes, surgery |
| Complications | Skin irritation, social embarrassment, aspiration pneumonia | Esophagitis, Barrett's esophagus, increased cancer risk |
Introduction to Sialorrhea
Sialorrhea, characterized by excessive saliva production or impaired clearance, often results from neurological disorders, medications, or local oral issues. Gastroesophageal Reflux Disease (GERD) can exacerbate sialorrhea by stimulating salivary glands through acid reflux, intensifying symptoms. Understanding the pathophysiology of sialorrhea independent of GERD aids in targeted management and treatment strategies.
Understanding Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD) is a chronic digestive disorder characterized by the backflow of stomach acid into the esophagus, causing symptoms such as heartburn, regurgitation, and dysphagia. Unlike sialorrhea, which involves excessive saliva production often due to neurological conditions or medications, GERD primarily affects the lower esophageal sphincter's function, leading to mucosal irritation and inflammation. Understanding GERD's pathophysiology is crucial for differentiating it from sialorrhea, as management strategies differ, focusing on acid suppression and lifestyle modification for GERD versus salivary control techniques for sialorrhea.
Relationship Between Sialorrhea and GERD
Sialorrhea, characterized by excessive saliva production, frequently correlates with Gastroesophageal Reflux Disease (GERD) due to reflux-induced esophageal irritation triggering increased salivary secretion as a protective mechanism. Studies report that patients with GERD often experience heightened sialorrhea, which serves to neutralize acid and facilitate esophageal clearance. Understanding this relationship improves clinical management strategies by addressing both excessive salivation and underlying reflux pathology.
Sialorrhea: Etiology and Risk Factors
Sialorrhea, characterized by excessive saliva production or impaired clearance, often stems from neurological disorders such as Parkinson's disease, cerebral palsy, and amyotrophic lateral sclerosis, which disrupt normal swallowing mechanisms. Gastroesophageal Reflux Disease (GERD) can exacerbate sialorrhea by irritating the esophagus and triggering increased salivary secretion as a protective response. Key risk factors for sialorrhea include neurodegenerative conditions, medication side effects (e.g., clozapine), and anatomical abnormalities affecting oral or pharyngeal structures.
Clinical Presentation: Sialorrhea vs. GERD-Associated Sialorrhea
Sialorrhea presents as excessive saliva production or impaired clearance leading to drooling, often linked to neurological conditions such as Parkinson's disease or cerebral palsy. GERD-associated sialorrhea manifests with hypersalivation triggered by acid reflux irritating the esophagus and oropharynx, causing increased swallowing and saliva secretion as a protective response. Clinically, GERD-related sialorrhea frequently coexists with symptoms like heartburn, regurgitation, and chronic cough, distinguishing it from isolated sialorrhea which primarily involves oral motor dysfunction without gastrointestinal symptoms.
Diagnostic Strategies for Sialorrhea and GERD
Diagnostic strategies for sialorrhea and gastroesophageal reflux disease (GERD) involve a combination of clinical evaluation and specialized testing. For sialorrhea, assessment includes thorough history taking, physical examination focusing on salivary gland function, and objective measures such as the Drooling Severity and Frequency Scale or sialometry to quantify saliva production. GERD diagnosis often relies on symptom assessment, esophageal pH monitoring, and endoscopic evaluation to detect mucosal damage, enabling differentiation between primary sialorrhea and saliva hypersalivation secondary to acid reflux.
Differential Diagnosis: Sialorrhea vs. Other Conditions
Differential diagnosis between Sialorrhea associated with Gastroesophageal Reflux Disease (GERD) and isolated Sialorrhea hinges on identifying underlying etiologies such as esophageal acid exposure in GERD, which stimulates excessive salivary production as a protective mechanism. Unlike isolated Sialorrhea, which may result from neurological disorders, medication side effects, or oral-motor dysfunction, GERD-related Sialorrhea often presents with accompanying symptoms like heartburn, regurgitation, and dysphagia. Accurate differentiation requires comprehensive clinical evaluation, including patient history, pH monitoring, and esophageal manometry to effectively tailor management strategies.
Treatment Approaches for Sialorrhea
Treatment approaches for sialorrhea vary depending on its underlying cause, with Gastroesophageal Reflux Disease (GERD) often necessitating a combined management strategy to address acid reflux and excessive saliva production. Pharmacological options such as anticholinergic drugs are commonly used to reduce saliva secretion, while botulinum toxin injections provide targeted relief by inhibiting salivary gland activity. In contrast, idiopathic sialorrhea may respond well to behavioral therapies or surgical interventions like duct ligation or gland excision when conservative treatments fail.
Management of Sialorrhea in GERD Patients
Management of sialorrhea in GERD patients involves addressing both excessive salivation and reflux symptoms to prevent aspiration and improve quality of life. Proton pump inhibitors (PPIs) and lifestyle modifications reduce acid exposure, while anticholinergic agents or botulinum toxin injections target salivary gland hyperactivity. Coordination of gastroenterology and otolaryngology care is essential to optimize treatment outcomes and minimize complications.
Prognosis and Patient Outcomes
Sialorrhea associated with Gastroesophageal Reflux Disease (GERD) often indicates a more complex clinical prognosis due to chronic esophageal irritation and increased saliva production as a compensatory mechanism. Patient outcomes in GERD-related sialorrhea frequently require integrated treatment targeting both reflux control and saliva management, leading to improved symptomatic relief and reduced risk of aspiration pneumonia. In contrast, sialorrhea without GERD is typically linked to neurological disorders or medication side effects and may have a more variable prognosis depending on the underlying cause and response to therapy.
Sialorrhea and Gastroesophageal Reflux Disease (GERD) Infographic
 libterm.com
libterm.com