Opportunistic behavior often involves taking advantage of situations without regard for ethical considerations, which can impact trust and relationships in both personal and professional settings. Understanding the characteristics and consequences of opportunistic actions can help you make informed decisions and protect your interests. Explore the rest of the article to learn how to identify opportunistic behavior and navigate its challenges effectively.
Table of Comparison
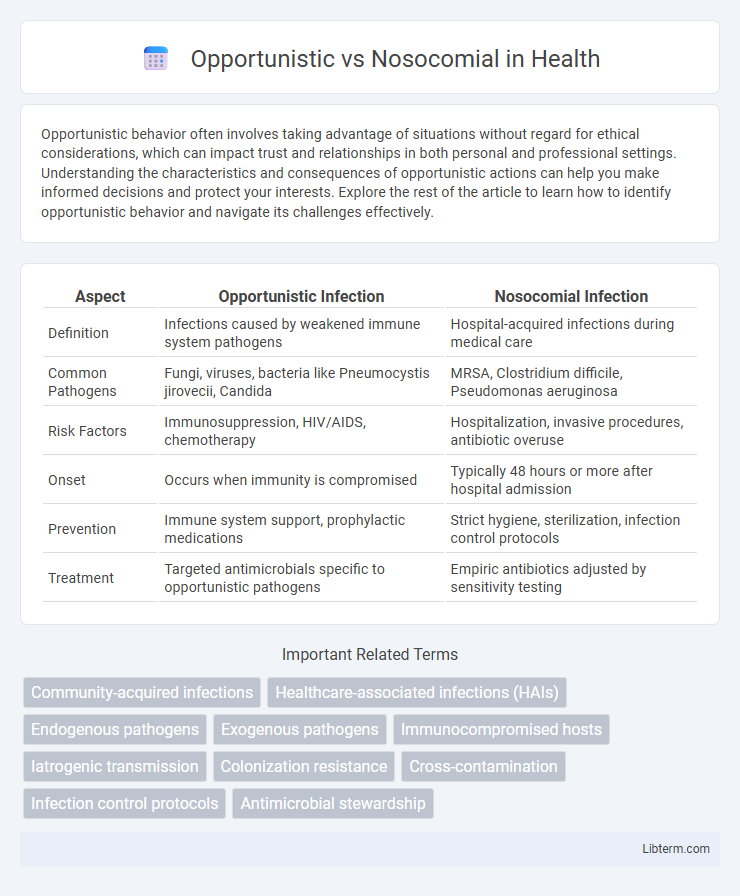
| Aspect | Opportunistic Infection | Nosocomial Infection |
|---|---|---|
| Definition | Infections caused by weakened immune system pathogens | Hospital-acquired infections during medical care |
| Common Pathogens | Fungi, viruses, bacteria like Pneumocystis jirovecii, Candida | MRSA, Clostridium difficile, Pseudomonas aeruginosa |
| Risk Factors | Immunosuppression, HIV/AIDS, chemotherapy | Hospitalization, invasive procedures, antibiotic overuse |
| Onset | Occurs when immunity is compromised | Typically 48 hours or more after hospital admission |
| Prevention | Immune system support, prophylactic medications | Strict hygiene, sterilization, infection control protocols |
| Treatment | Targeted antimicrobials specific to opportunistic pathogens | Empiric antibiotics adjusted by sensitivity testing |
Understanding Opportunistic Infections
Opportunistic infections occur when normally harmless pathogens exploit a weakened immune system, often seen in individuals with HIV/AIDS, cancer, or following organ transplantation. These infections differ from nosocomial infections, which are contracted in healthcare settings regardless of immune status. Understanding opportunistic infections involves recognizing their reliance on compromised immunity and the range of pathogens, including fungi, bacteria, and viruses, that cause severe illness in vulnerable patients.
Defining Nosocomial Infections
Nosocomial infections, also known as hospital-acquired infections (HAIs), are infections contracted by patients during their stay in healthcare facilities, typically emerging 48 hours or more after admission. These infections often involve pathogens like Staphylococcus aureus, including methicillin-resistant strains (MRSA), and can result from invasive procedures, contaminated medical devices, or inadequate sterilization. Opportunistic infections differ by primarily affecting immunocompromised individuals, whereas nosocomial infections emphasize the healthcare environment as the source of pathogen exposure.
Key Differences Between Opportunistic and Nosocomial Infections
Opportunistic infections occur when normally harmless pathogens exploit a weakened immune system, while nosocomial infections are acquired specifically within healthcare settings such as hospitals. Opportunistic infections often stem from endogenous flora or environmental microbes, contrasting with nosocomial infections that typically involve drug-resistant bacteria like MRSA or Clostridium difficile. The critical difference lies in their origin and context: opportunistic infections target immunocompromised patients broadly, whereas nosocomial infections are linked to medical interventions and hospital environments.
Common Opportunistic Pathogens
Common opportunistic pathogens include Candida albicans, Pseudomonas aeruginosa, and Cytomegalovirus, which primarily infect immunocompromised individuals. These pathogens exploit weakened immune defenses, unlike nosocomial infections that arise from hospital environments regardless of immune status. Understanding the virulence factors and resistance mechanisms of these opportunistic microbes is crucial for targeted antimicrobial therapy and infection control.
Frequent Nosocomial Infection Sources
Frequent nosocomial infection sources include contaminated medical devices, surgical instruments, and hospital surfaces, which harbor pathogens like Staphylococcus aureus and Pseudomonas aeruginosa. Opportunistic infections often arise from these sources when patients have weakened immune systems or invasive procedures breach natural barriers. Understanding the distinction highlights the importance of strict sterilization protocols and infection control measures in healthcare settings.
Risk Factors for Opportunistic Infections
Immunocompromised conditions such as HIV/AIDS, chemotherapy, organ transplantation, and prolonged corticosteroid use significantly increase the risk of opportunistic infections. Environmental factors including exposure to pathogens in healthcare settings or contaminated surroundings also contribute to susceptibility. Unlike nosocomial infections, which chiefly occur due to hospital-acquired pathogens, opportunistic infections arise primarily from the host's weakened immune defenses.
Hospital Settings and Nosocomial Infection Risks
Nosocomial infections, also known as hospital-acquired infections (HAIs), occur due to exposure to pathogens within healthcare settings, posing significant risks to immunocompromised patients. Opportunistic infections exploit weakened immune defenses and are frequently associated with prolonged hospital stays, invasive procedures, and use of medical devices such as catheters or ventilators. Implementing strict hygiene protocols, surveillance, and antimicrobial stewardship is essential to mitigate the transmission of nosocomial pathogens like MRSA, Clostridium difficile, and multidrug-resistant Gram-negative bacteria.
Prevention Strategies for Opportunistic Infections
Effective prevention strategies for opportunistic infections primarily involve strengthening the immune system through antiretroviral therapy in HIV patients and prophylactic antimicrobial treatments tailored to individual risk factors. Maintaining strict hygiene practices, avoiding exposure to known environmental pathogens, and timely vaccination against preventable diseases significantly reduce infection rates. Regular monitoring of immune status and early intervention remain critical components in minimizing the incidence of opportunistic infections.
Nosocomial Infection Control Measures
Nosocomial infections, also known as hospital-acquired infections (HAIs), require stringent infection control measures such as hand hygiene protocols, sterilization of medical equipment, and isolation of infected patients to prevent cross-contamination. Implementation of antimicrobial stewardship programs reduces the emergence of resistant pathogens, while regular surveillance and environmental cleaning are critical in identifying and mitigating infection sources. Effective nosocomial infection control ultimately decreases patient morbidity, healthcare costs, and the spread of multidrug-resistant organisms in clinical settings.
Clinical Outcomes and Management Approaches
Opportunistic infections arise primarily in immunocompromised patients, leading to varied clinical outcomes depending on the host's immune status and pathogen virulence, often requiring targeted antimicrobial therapy and immune system support. Nosocomial infections, acquired in healthcare settings, frequently involve multidrug-resistant organisms, complicating treatment and prolonging hospital stays, thus necessitating stringent infection control measures and antibiotic stewardship. Effective management approaches differ as opportunistic infections focus on correcting immune deficits, whereas nosocomial infections demand prevention strategies, rapid diagnosis, and tailored antimicrobial regimens to reduce morbidity and mortality.
Opportunistic Infographic
 libterm.com
libterm.com