An outbreak occurs when a sudden increase in disease cases spreads rapidly within a specific geographic area or population. Understanding the causes, transmission methods, and preventive measures is crucial to controlling its impact and safeguarding public health. Explore the following article to learn how you can protect yourself and your community during an outbreak.
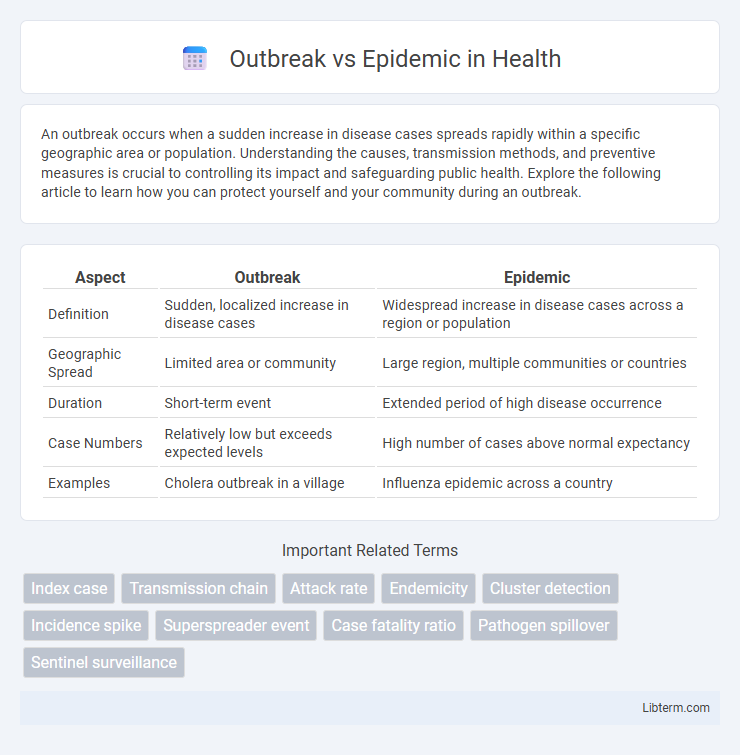
Table of Comparison
| Aspect | Outbreak | Epidemic |
|---|---|---|
| Definition | Sudden, localized increase in disease cases | Widespread increase in disease cases across a region or population |
| Geographic Spread | Limited area or community | Large region, multiple communities or countries |
| Duration | Short-term event | Extended period of high disease occurrence |
| Case Numbers | Relatively low but exceeds expected levels | High number of cases above normal expectancy |
| Examples | Cholera outbreak in a village | Influenza epidemic across a country |
Defining Outbreak and Epidemic
An outbreak refers to the sudden occurrence of cases of a disease in a specific community or region, often confined to a limited geographic area or population, while an epidemic denotes a more widespread increase in disease cases that exceeds the expected number within a larger geographic area or population over a given period. Both terms relate to disease prevalence but differ in scale and intensity, with outbreaks potentially escalating into epidemics if uncontrolled. Understanding these definitions is critical for effective public health response and containment strategies.
Key Similarities and Differences
Outbreak and epidemic both refer to the sudden increase in the number of disease cases in a specific population or area, often caused by the rapid spread of infectious agents. The key difference lies in scale and duration: an outbreak is typically more localized and short-term, affecting a limited area or population, whereas an epidemic covers a broader geographic region and can last longer. Both require public health interventions to control and prevent further transmission, emphasizing timely identification and response to minimize impact.
Causes of Outbreaks
Outbreaks are typically caused by a sudden increase in the presence of pathogens due to factors such as contaminated food or water, close contact in crowded settings, or zoonotic transmission from animals to humans. Environmental changes, poor sanitation, and lack of vaccination can also trigger outbreaks by facilitating rapid pathogen spread. These localized surges in infection contrast with epidemics, which represent larger-scale outbreaks often influenced by broader social and ecological dynamics.
Causes of Epidemics
Epidemics occur due to a confluence of factors including pathogen evolution, increased human susceptibility, and environmental changes that facilitate transmission. Causes such as population density, poor sanitation, and global travel accelerate the spread of infectious agents beyond endemic levels. Understanding these drivers is critical for designing effective public health interventions to contain outbreaks before they escalate into epidemics.
Scale and Severity Comparison
An outbreak refers to a sudden increase in cases of a disease within a localized area, often limited in scale and duration, while an epidemic involves a more extensive spread affecting a larger population across regions or countries. The severity of an epidemic is typically higher due to its broader impact on public health systems, increased transmission rates, and potential for significant morbidity and mortality. Metrics such as infection rate, geographic spread, and population affected help distinguish between outbreak and epidemic severity and scale.
Detection and Identification
Detection of an outbreak involves recognizing a sudden increase in cases within a specific area or population, often through surveillance systems and laboratory confirmation. Identification of an epidemic requires confirming widespread transmission beyond initial clusters, typically using epidemiological data and case mapping to assess the scale and impact. Accurate and timely detection and identification rely on robust reporting mechanisms, diagnostic testing, and real-time data analysis to implement effective public health interventions.
Common Examples of Outbreaks
Common examples of outbreaks include localized incidents of diseases such as measles in schools, foodborne illnesses like salmonella from contaminated products, and seasonal influenza clusters in communities. Outbreaks often involve a sudden increase in cases within a specific geographic area or population, distinguishing them from broader epidemics that cover larger regions. Tracking these outbreaks requires rapid response and targeted public health interventions to prevent escalation.
Historical Epidemics in Perspective
Historical epidemics like the Black Death and the 1918 Spanish flu transformed societies by causing widespread morbidity and mortality on a global scale, distinguishing them from localized outbreaks such as the 2014 Ebola flare-ups in West Africa. Epidemics represent an extraordinary increase in disease incidence across a large population or region, whereas outbreaks are confined to smaller, specific geographic locations or communities. Understanding these distinctions contextualizes public health responses and the socio-economic impacts observed during significant events such as the Cholera epidemics in 19th century Europe and the smallpox crises in North America.
Strategies for Prevention and Control
Outbreak and epidemic prevention strategies emphasize early detection through surveillance systems and rapid reporting to contain pathogen spread. Implementing vaccination campaigns, promoting hygiene practices, and enforcing quarantine measures reduce transmission rates effectively. Public health education and resource allocation for medical infrastructure strengthen community resilience against contagious disease surges.
Importance of Public Health Response
Efficient public health response is crucial in controlling outbreaks and epidemics to prevent widespread disease transmission and minimize morbidity and mortality. Rapid identification, surveillance, and timely intervention, such as vaccination campaigns and quarantine measures, are essential to contain pathogen spread. Strengthening healthcare infrastructure and ensuring effective communication with the public enhance resilience against future outbreaks and epidemics.
Outbreak Infographic
 libterm.com
libterm.com