Drug reactions occur when your body responds unexpectedly to a medication, ranging from mild symptoms like rashes to severe allergic responses. Understanding the signs and mechanisms behind these reactions is crucial for safe treatment and prompt medical intervention. Explore the full article to learn how to recognize, manage, and prevent adverse drug reactions effectively.
Table of Comparison
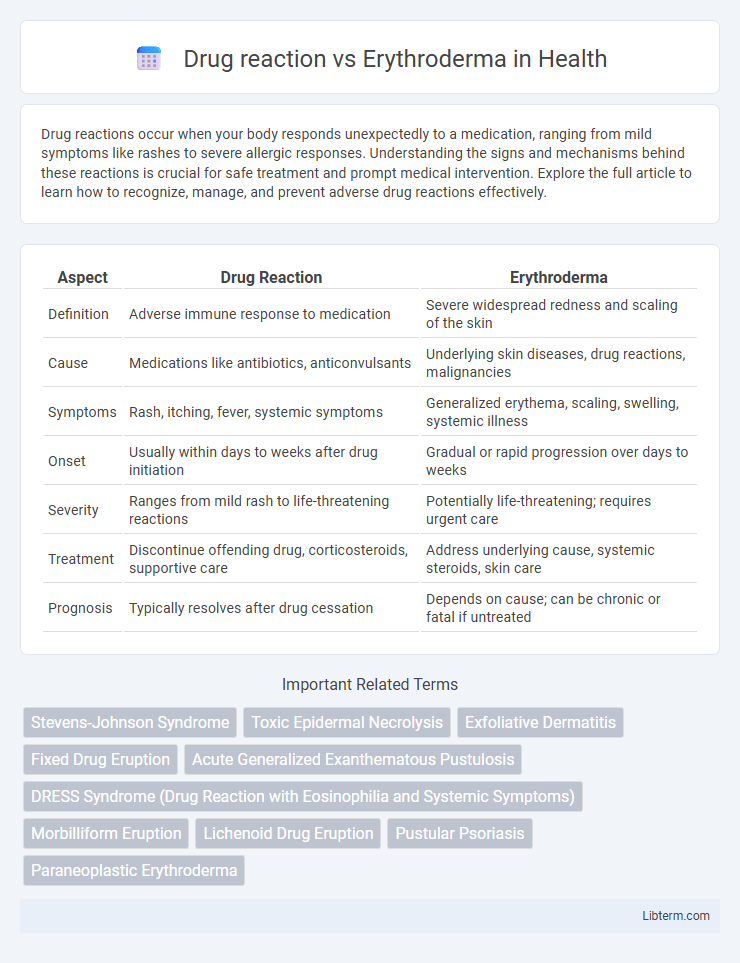
| Aspect | Drug Reaction | Erythroderma |
|---|---|---|
| Definition | Adverse immune response to medication | Severe widespread redness and scaling of the skin |
| Cause | Medications like antibiotics, anticonvulsants | Underlying skin diseases, drug reactions, malignancies |
| Symptoms | Rash, itching, fever, systemic symptoms | Generalized erythema, scaling, swelling, systemic illness |
| Onset | Usually within days to weeks after drug initiation | Gradual or rapid progression over days to weeks |
| Severity | Ranges from mild rash to life-threatening reactions | Potentially life-threatening; requires urgent care |
| Treatment | Discontinue offending drug, corticosteroids, supportive care | Address underlying cause, systemic steroids, skin care |
| Prognosis | Typically resolves after drug cessation | Depends on cause; can be chronic or fatal if untreated |
Introduction to Drug Reaction and Erythroderma
Drug reaction refers to adverse responses triggered by medications, often presenting with skin manifestations ranging from mild rashes to severe hypersensitivity syndromes. Erythroderma, also known as exfoliative dermatitis, is characterized by widespread redness and scaling involving over 90% of the body surface area, frequently caused by drug reactions, underlying dermatoses, or malignancies. Both conditions require prompt identification due to the potential for systemic involvement and significant morbidity.
Definitions and Key Differences
Drug reaction refers to an adverse response triggered by medication intake, often manifesting as rash, fever, or systemic symptoms. Erythroderma is a severe dermatological condition characterized by widespread redness and scaling covering more than 90% of the body surface, often resulting from underlying skin diseases or drug reactions. The key difference lies in erythroderma being a clinical syndrome involving extensive skin involvement, whereas drug reactions may present with a variety of skin and systemic symptoms without necessarily causing widespread exfoliative dermatitis.
Causes of Drug Reactions
Drug reactions are caused by hypersensitivity to medications such as antibiotics, anticonvulsants, nonsteroidal anti-inflammatory drugs (NSAIDs), and allopurinol. These reactions can manifest as mild rashes to severe systemic involvement. Erythroderma, often triggered by prolonged drug exposure or discontinuation, is a severe and widespread skin condition that may result from such adverse drug reactions.
Common Triggers of Erythroderma
Erythroderma is frequently triggered by drug reactions involving antibiotics, anticonvulsants, and allopurinol, which provoke widespread skin inflammation. Common non-drug triggers include psoriasis, atopic dermatitis, and cutaneous T-cell lymphoma, leading to generalized erythema and scaling. Identification of the underlying cause is critical to managing erythroderma effectively and preventing complications.
Clinical Presentation: Drug Reaction vs Erythroderma
Drug reactions typically present with acute onset of widespread rash, fever, and systemic symptoms such as eosinophilia and lymphadenopathy, often accompanied by mucosal involvement and pruritus. Erythroderma manifests as generalized erythema and scaling over more than 90% of the body surface area, frequently associated with underlying chronic dermatoses or malignancies, and may include thickened skin, alopecia, and nail changes. Differentiating clinical features include the rapid progression and systemic hypersensitivity markers in drug reactions versus the chronic, persistent scaling and extensive skin barrier disruption seen in erythroderma.
Diagnostic Approaches
Diagnostic approaches for drug reactions involve detailed patient history, identification of recent medication exposure, and skin biopsy to detect immune-mediated inflammation. Erythroderma diagnosis requires assessment of underlying causes, including psoriasis, atopic dermatitis, or drug-induced origins, supported by clinical examination and histopathology. Laboratory tests such as complete blood count, liver function tests, and patch testing assist in distinguishing between drug reactions and erythroderma etiologies.
Histopathological Features
Drug reactions typically present with a mixed inflammatory infiltrate in the dermis, including eosinophils and interface dermatitis, while erythroderma commonly shows psoriasiform hyperplasia and spongiosis. Histopathological features of drug reactions often reveal necrotic keratinocytes and a perivascular lymphocytic infiltrate with eosinophils, whereas erythroderma demonstrates diffuse epidermal involvement with thickening and parakeratosis. Differentiating these conditions microscopically relies on identifying the predominance of eosinophils and necrosis in drug reactions versus the widespread epidermal hyperplasia characteristic of erythroderma.
Management and Treatment Strategies
Management of drug reaction involves immediate discontinuation of the offending medication, supportive care with antihistamines, corticosteroids, and close monitoring for systemic involvement. Erythroderma treatment requires identification of underlying causes, aggressive skin care with emollients, systemic corticosteroids or immunosuppressants, and hospitalization in severe cases to prevent complications like infection and fluid imbalance. Both conditions necessitate careful patient evaluation and tailored therapeutic approaches to ensure rapid resolution and avoid progression.
Prognosis and Complications
Drug reaction-induced erythroderma often presents a variable prognosis dependent on the severity and promptness of treatment, with potential complications including secondary infections, fluid and electrolyte imbalances, and systemic organ involvement. Erythroderma unrelated to drugs typically carries a prognosis influenced by the underlying cause, such as psoriasis or cutaneous T-cell lymphoma, and may lead to complications like thermoregulatory failure, high-output cardiac failure, and severe skin barrier disruption. Early identification and management of the causative factor are critical to reducing morbidity and mortality in both drug reaction-associated and non-drug erythroderma cases.
Prevention and Patient Education
Preventing drug reactions involves thorough patient history assessment, careful medication selection, and monitoring for early symptoms, emphasizing avoidance of known allergens and cross-reactive drugs. Patient education should focus on recognizing initial signs of adverse reactions, adherence to prescribed dosages, and immediate reporting of skin changes, especially redness and scaling typical of erythroderma. Clear communication about potential risks and prompt medical consultation helps reduce severity and prevents progression to life-threatening conditions.
Drug reaction Infographic
 libterm.com
libterm.com