Hirsutism, characterized by excessive hair growth in women, is a common symptom of Polycystic Ovary Syndrome (PCOS), a hormonal disorder affecting reproductive-aged women. This condition results from elevated androgen levels, leading to symptoms like irregular periods, acne, and unwanted hair growth, impacting your self-confidence and health. Explore the article to understand the causes, diagnosis, and effective treatments for managing hirsutism associated with PCOS.
Table of Comparison
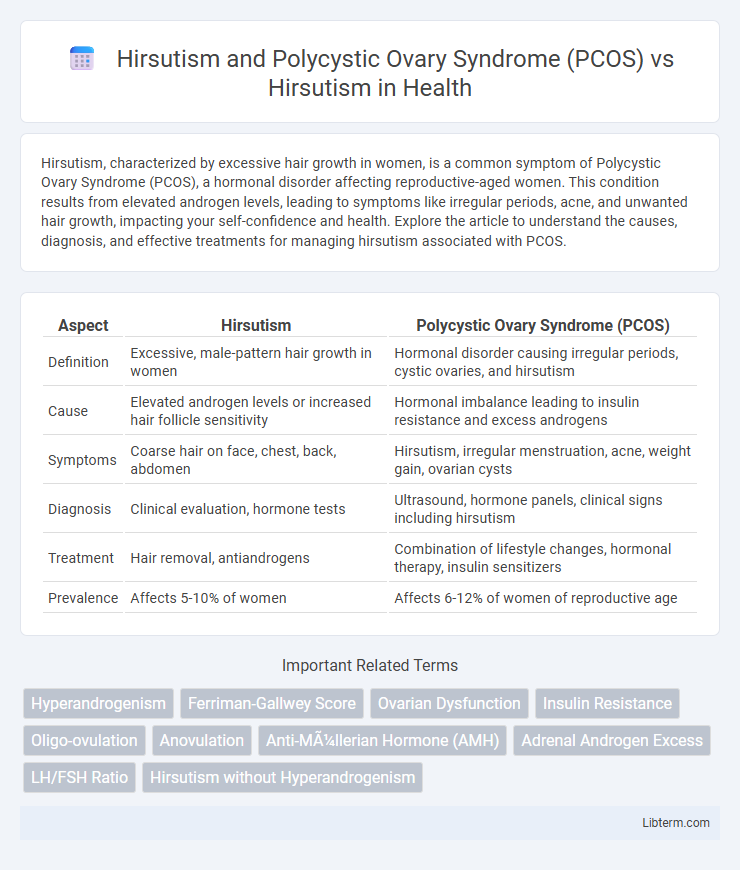
| Aspect | Hirsutism | Polycystic Ovary Syndrome (PCOS) |
|---|---|---|
| Definition | Excessive, male-pattern hair growth in women | Hormonal disorder causing irregular periods, cystic ovaries, and hirsutism |
| Cause | Elevated androgen levels or increased hair follicle sensitivity | Hormonal imbalance leading to insulin resistance and excess androgens |
| Symptoms | Coarse hair on face, chest, back, abdomen | Hirsutism, irregular menstruation, acne, weight gain, ovarian cysts |
| Diagnosis | Clinical evaluation, hormone tests | Ultrasound, hormone panels, clinical signs including hirsutism |
| Treatment | Hair removal, antiandrogens | Combination of lifestyle changes, hormonal therapy, insulin sensitizers |
| Prevalence | Affects 5-10% of women | Affects 6-12% of women of reproductive age |
Understanding Hirsutism: Definition and Causes
Hirsutism is characterized by excessive, unwanted male-pattern hair growth in women, primarily caused by increased androgen levels or heightened sensitivity of hair follicles to androgens. Polycystic Ovary Syndrome (PCOS), a common endocrine disorder affecting 6-12% of women of reproductive age, is a primary underlying cause of hirsutism due to elevated androgens like testosterone. Understanding the hormonal imbalances and genetic factors involved is crucial for accurate diagnosis and targeted treatment of hirsutism associated with PCOS versus other etiologies.
Polycystic Ovary Syndrome (PCOS): Overview and Symptoms
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder affecting 6-12% of women of reproductive age, characterized by elevated androgens leading to symptoms such as hirsutism, irregular menstrual cycles, and polycystic ovaries visible on ultrasound. Hirsutism, a common symptom of PCOS, manifests as excessive, coarse hair growth in androgen-sensitive areas like the face, chest, and back. The presence of PCOS significantly increases the risk of metabolic issues including insulin resistance, obesity, and type 2 diabetes, distinguishing it from isolated hirsutism cases.
Hirsutism in PCOS: Connection and Prevalence
Hirsutism in Polycystic Ovary Syndrome (PCOS) is a common manifestation caused by androgen excess, affecting approximately 70% of women with PCOS. This condition results in excessive terminal hair growth in typically male-pattern areas such as the face, chest, and back, driven by elevated levels of testosterone and other androgens. Understanding the link between hirsutism and PCOS is crucial for accurate diagnosis and targeted treatments that address both hormonal imbalance and cosmetic concerns.
Hirsutism Without PCOS: Other Underlying Conditions
Hirsutism without Polycystic Ovary Syndrome (PCOS) can result from various underlying conditions such as adrenal hyperplasia, Cushing's syndrome, or androgen-secreting tumors. These alternative causes require specific diagnostic evaluations including hormonal assays and imaging studies to differentiate from PCOS-induced hirsutism. Understanding non-PCOS etiologies of hirsutism is crucial for targeted treatment and effective management of the hyperandrogenic symptoms.
Key Differences Between PCOS-Related Hirsutism and Isolated Hirsutism
Hirsutism in Polycystic Ovary Syndrome (PCOS) typically presents with other endocrine abnormalities such as irregular menstrual cycles, insulin resistance, and elevated androgen levels, whereas isolated hirsutism occurs without these systemic manifestations. PCOS-related hirsutism often involves a multifactorial pathogenesis including hyperandrogenism and metabolic syndrome, while isolated hirsutism usually stems from idiopathic or adrenal causes without underlying systemic hormonal imbalance. Diagnostic approaches for PCOS-related hirsutism emphasize assessing ovulatory function and metabolic parameters, contrasting with isolated hirsutism which requires evaluation of localized hair growth patterns and exclusion of secondary endocrine disorders.
Diagnostic Criteria: Hirsutism vs PCOS-Associated Hirsutism
Hirsutism is characterized by excessive terminal hair growth in androgen-dependent areas, typically assessed using the Ferriman-Gallwey score with a threshold of >=8 indicating clinically significant hirsutism. Polycystic Ovary Syndrome (PCOS)-associated hirsutism combines this clinical sign with diagnostic criteria including hyperandrogenism, oligo/anovulation, and polycystic ovarian morphology per the Rotterdam criteria. Differentiating hirsutism alone from PCOS-associated hirsutism requires evaluating biochemical hyperandrogenism and ovarian ultrasound findings alongside clinical assessment.
Hormonal Imbalances: Androgens in PCOS and Isolated Hirsutism
Hirsutism in Polycystic Ovary Syndrome (PCOS) is primarily driven by elevated androgen levels, including testosterone and androstenedione, resulting from ovarian and adrenal hyperactivity. Isolated hirsutism often involves normal systemic androgen concentrations with increased peripheral sensitivity of hair follicles to androgens or minor local androgen production. Understanding these hormonal imbalances is crucial for differentiating PCOS-associated hirsutism from idiopathic or isolated forms, guiding targeted therapeutic approaches.
Treatment Approaches: Comparative Management Strategies
Treatment approaches for hirsutism associated with Polycystic Ovary Syndrome (PCOS) primarily involve hormonal therapies such as combined oral contraceptives and anti-androgens like spironolactone to reduce androgen levels and manage symptoms. Isolated hirsutism without PCOS often requires topical treatments like eflornithine cream and physical hair removal methods, with hormonal therapy considered only if underlying endocrine abnormalities are detected. Lifestyle modifications, including weight loss and insulin-sensitizing agents like metformin, are integral to PCOS-related hirsutism management, addressing both metabolic and dermatologic symptoms simultaneously.
Impact on Quality of Life: PCOS vs Non-PCOS Hirsutism
Hirsutism associated with Polycystic Ovary Syndrome (PCOS) often leads to more severe physical symptoms and psychological distress compared to non-PCOS hirsutism, significantly impacting quality of life. Women with PCOS-related hirsutism report higher levels of anxiety, depression, and body image concerns due to the systemic hormonal imbalances and metabolic complications characteristic of PCOS. In contrast, non-PCOS hirsutism may present with fewer systemic symptoms, resulting in a comparatively lesser negative effect on emotional well-being and daily functioning.
Early Detection, Prevention, and Long-Term Outlook
Early detection of hirsutism linked to Polycystic Ovary Syndrome (PCOS) involves identifying hormonal imbalances such as elevated androgens and irregular menstrual cycles through blood tests and ultrasound imaging. Preventive strategies emphasize lifestyle modifications, including weight management and insulin resistance control, which can reduce symptom severity and metabolic risks associated with PCOS-induced hirsutism. The long-term outlook improves with timely medical interventions like anti-androgens and oral contraceptives, decreasing the risk of complications such as infertility, type 2 diabetes, and cardiovascular disease.
Hirsutism and Polycystic Ovary Syndrome (PCOS) Infographic
 libterm.com
libterm.com