Cholelithiasis is the formation of gallstones within the gallbladder, which can cause pain, nausea, and digestive issues. Risk factors include obesity, rapid weight loss, and certain medical conditions that affect bile composition. Learn more about symptoms, diagnosis, and treatment options to manage your health effectively in the rest of this article.
Table of Comparison
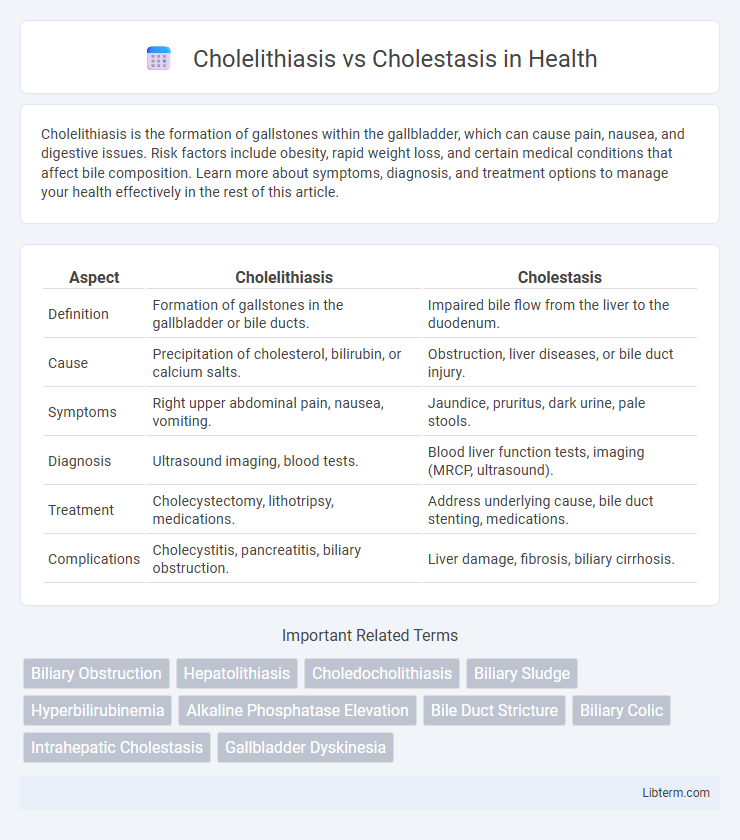
| Aspect | Cholelithiasis | Cholestasis |
|---|---|---|
| Definition | Formation of gallstones in the gallbladder or bile ducts. | Impaired bile flow from the liver to the duodenum. |
| Cause | Precipitation of cholesterol, bilirubin, or calcium salts. | Obstruction, liver diseases, or bile duct injury. |
| Symptoms | Right upper abdominal pain, nausea, vomiting. | Jaundice, pruritus, dark urine, pale stools. |
| Diagnosis | Ultrasound imaging, blood tests. | Blood liver function tests, imaging (MRCP, ultrasound). |
| Treatment | Cholecystectomy, lithotripsy, medications. | Address underlying cause, bile duct stenting, medications. |
| Complications | Cholecystitis, pancreatitis, biliary obstruction. | Liver damage, fibrosis, biliary cirrhosis. |
Introduction to Cholelithiasis and Cholestasis
Cholelithiasis is the formation of gallstones within the gallbladder, often causing biliary colic, nausea, and potential obstruction of bile flow. Cholestasis refers to impaired bile flow from the liver to the duodenum, leading to accumulation of bile acids and jaundice. Both conditions disrupt normal bile physiology but differ in etiology, with cholelithiasis primarily caused by supersaturation of bile components and cholestasis resulting from hepatocellular or extrahepatic bile duct dysfunction.
Definition and Overview
Cholelithiasis refers to the formation of gallstones within the gallbladder or bile ducts, causing obstruction and pain due to hardened deposits of bile components. Cholestasis is a condition characterized by impaired bile flow from the liver to the duodenum, leading to bile accumulation and liver damage. While cholelithiasis often results in mechanical blockage, cholestasis encompasses a broader spectrum including intrahepatic and extrahepatic causes affecting bile secretion or transport.
Etiology: Causes and Risk Factors
Cholelithiasis is primarily caused by the crystallization of bile components, such as cholesterol or bilirubin, often due to factors like obesity, rapid weight loss, pregnancy, and genetic predisposition. Cholestasis results from impaired bile flow, which may arise from intrahepatic causes like liver diseases (e.g., hepatitis, cirrhosis) or extrahepatic obstruction such as gallstones, tumors, or bile duct strictures. Risk factors for cholelithiasis include female gender, age over 40, and metabolic syndrome, while cholestasis risk factors depend on the underlying condition but commonly include liver dysfunction and biliary tract obstruction.
Pathophysiology: How They Differ
Cholelithiasis involves the formation of gallstones primarily due to cholesterol supersaturation, bile stasis, and gallbladder hypomotility, leading to mechanical obstruction and inflammation within the biliary system. Cholestasis results from impaired bile flow caused by intrahepatic or extrahepatic bile duct obstruction, hepatocellular dysfunction, or transporter defects, which disrupt bile secretion and lead to accumulation of bile acids and bilirubin in the liver. The key pathological difference lies in cholelithiasis being a mechanical obstruction due to solid concretions, while cholestasis is characterized by functional or structural bile flow impairment at the cellular or ductal level.
Clinical Presentation and Symptoms
Cholelithiasis commonly manifests with episodic right upper quadrant pain, often intense and colicky, accompanied by nausea and vomiting, especially after fatty meals. Cholestasis presents with persistent jaundice, pruritus, dark urine, and pale stools due to impaired bile flow and accumulation of bile salts in the bloodstream. Both conditions may exhibit elevated liver enzymes, but cholestasis uniquely causes marked increases in alkaline phosphatase and gamma-glutamyl transferase levels.
Diagnostic Approaches and Laboratory Findings
Cholelithiasis diagnosis primarily relies on abdominal ultrasound revealing gallstones within the gallbladder, combined with elevated liver enzymes such as alkaline phosphatase and gamma-glutamyl transferase (GGT) if biliary obstruction occurs. Cholestasis diagnosis involves laboratory findings of elevated serum bilirubin, especially direct (conjugated) bilirubin, along with markedly increased alkaline phosphatase and GGT levels, supported by imaging like magnetic resonance cholangiopancreatography (MRCP) to detect bile duct obstruction. Both conditions require differentiation using liver function tests (LFTs) and imaging studies to guide targeted clinical management.
Imaging Techniques for Differentiation
Ultrasound is the primary imaging technique to differentiate cholelithiasis from cholestasis, where cholelithiasis presents as echogenic foci with posterior acoustic shadowing within the gallbladder. Magnetic Resonance Cholangiopancreatography (MRCP) provides detailed visualization of the biliary tree, detecting bile duct obstructions characteristic of cholestasis without direct stone visualization. Computed Tomography (CT) may assist in identifying complications but is less sensitive than ultrasound and MRCP for distinguishing gallstones from biliary dilatation.
Treatment and Management Strategies
Cholelithiasis treatment primarily involves cholecystectomy or non-surgical options like ursodeoxycholic acid to dissolve small gallstones, while managing symptoms with pain control and hydration. Cholestasis management centers on addressing the underlying cause, such as bile duct obstruction or liver disease, with therapies including bile acid sequestrants, ursodeoxycholic acid, or surgical intervention to restore bile flow. Both conditions require careful monitoring of liver function tests and bile duct imaging to guide therapeutic decisions and prevent complications like cholangitis or biliary cirrhosis.
Complications and Prognosis
Cholelithiasis, characterized by gallstone formation, commonly leads to complications such as acute cholecystitis, biliary colic, and potential gallstone pancreatitis, with prognosis largely dependent on the occurrence of infection or obstruction. Cholestasis, involving impaired bile flow, can result in complications like biliary cirrhosis, fat-soluble vitamin deficiencies, and progressive liver damage, often leading to chronic liver disease if untreated. Prognosis in cholestasis varies with the underlying cause and duration, with early intervention crucial to prevent irreversible hepatic injury.
Prevention and Patient Education
Preventing cholelithiasis involves maintaining a healthy weight through balanced diet and regular exercise to reduce cholesterol saturation in bile, while avoiding rapid weight loss and high-fat diets that increase stone formation risk. Educating patients about cholestasis centers on recognizing symptoms such as jaundice and understanding the importance of timely medical evaluation and adherence to prescribed treatments to prevent liver damage. Emphasizing routine monitoring and lifestyle modifications helps manage underlying conditions contributing to both cholelithiasis and cholestasis.
Cholelithiasis Infographic
 libterm.com
libterm.com