Psoriasis is a chronic autoimmune condition characterized by the rapid buildup of skin cells, resulting in scaling, redness, and inflammation that can cause significant discomfort. Effective management involves understanding triggers, treatment options, and lifestyle adjustments to reduce flare-ups and improve skin health. Discover how you can better manage psoriasis and enhance your quality of life by reading the rest of this article.
Table of Comparison
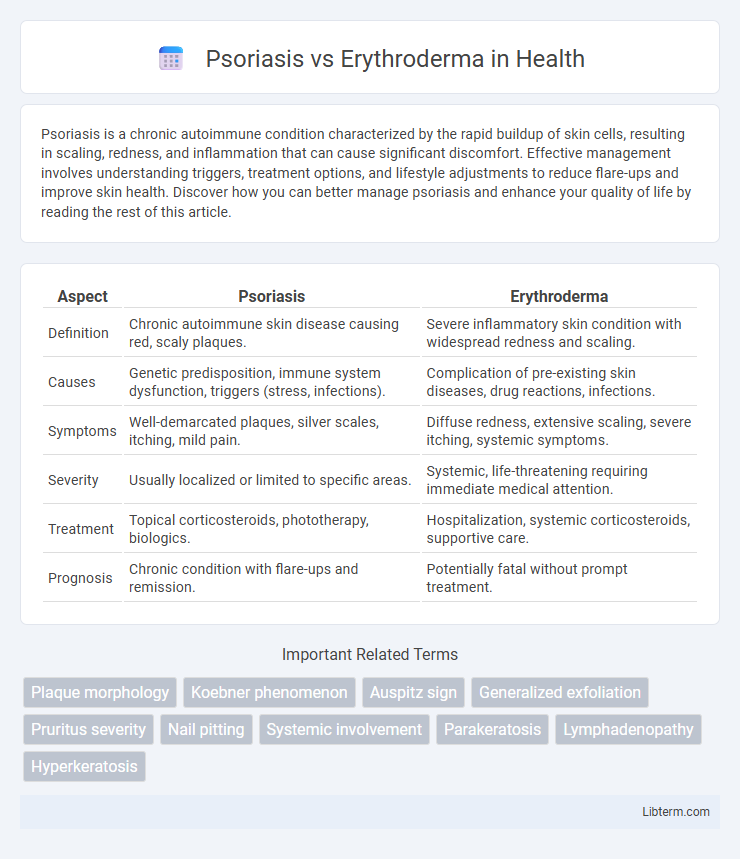
| Aspect | Psoriasis | Erythroderma |
|---|---|---|
| Definition | Chronic autoimmune skin disease causing red, scaly plaques. | Severe inflammatory skin condition with widespread redness and scaling. |
| Causes | Genetic predisposition, immune system dysfunction, triggers (stress, infections). | Complication of pre-existing skin diseases, drug reactions, infections. |
| Symptoms | Well-demarcated plaques, silver scales, itching, mild pain. | Diffuse redness, extensive scaling, severe itching, systemic symptoms. |
| Severity | Usually localized or limited to specific areas. | Systemic, life-threatening requiring immediate medical attention. |
| Treatment | Topical corticosteroids, phototherapy, biologics. | Hospitalization, systemic corticosteroids, supportive care. |
| Prognosis | Chronic condition with flare-ups and remission. | Potentially fatal without prompt treatment. |
Understanding Psoriasis: Overview and Causes
Psoriasis is a chronic autoimmune skin disorder characterized by rapid skin cell proliferation, leading to thick, scaly plaques predominantly on the elbows, knees, and scalp. Genetic predisposition, immune system dysfunction, and environmental triggers such as stress, infections, and certain medications contribute to its onset and exacerbation. Unlike erythroderma, which involves widespread skin inflammation and redness often resulting from severe psoriasis or other dermatological conditions, psoriasis primarily manifests as localized plaques with variable severity.
Erythroderma: Definition and Triggers
Erythroderma is a severe inflammatory skin condition characterized by widespread redness and scaling affecting over 90% of the body surface area. Common triggers include exacerbations of pre-existing skin diseases like psoriasis, drug reactions, and underlying malignancies. Prompt identification and treatment of these triggers are crucial to prevent systemic complications and improve patient outcomes.
Clinical Presentation: Psoriasis vs Erythroderma
Psoriasis typically presents with well-demarcated, erythematous plaques covered by silvery scales, primarily affecting extensor surfaces such as elbows and knees. Erythroderma, characterized by generalized erythema and scaling involving more than 90% of the body surface area, often indicates a severe inflammatory or drug-induced reaction and can be a complication of psoriasis itself. Unlike localized psoriatic plaques, erythroderma presents with widespread skin redness, edema, and potential systemic symptoms like fever and malaise, requiring urgent clinical evaluation.
Key Differences in Skin Manifestations
Psoriasis presents as well-demarcated, thick, silvery scales on erythematous plaques commonly found on extensor surfaces, while erythroderma involves widespread redness and scaling covering over 90% of the body surface area, often leading to skin exfoliation. Psoriasis lesions tend to be localized with chronic relapsing patterns, whereas erythroderma is an acute or chronic inflammatory condition causing diffuse skin involvement and systemic symptoms. The scale in psoriasis is typically dry and adherent, contrasting with the generalized erythema and shedding seen in erythroderma, reflecting distinct pathological processes.
Diagnostic Approaches for Psoriasis and Erythroderma
Diagnostic approaches for psoriasis primarily involve clinical examination of characteristic plaques with silvery scales, supported by skin biopsy revealing epidermal hyperplasia and parakeratosis. Erythroderma diagnosis requires comprehensive evaluation of widespread erythema covering over 90% of the body surface, often necessitating histopathological analysis to differentiate underlying causes like drug reactions, cutaneous T-cell lymphoma, or severe psoriasis. Dermoscopy, laboratory tests including complete blood count and liver function tests, and patient history are critical in distinguishing erythroderma from generalized psoriasis flare-ups and other dermatoses.
Risk Factors: Who Is More Prone?
Psoriasis primarily affects individuals with a genetic predisposition, immune system disorders, and those exposed to triggers like stress, infections, or certain medications. Erythroderma risk is higher in patients with severe underlying skin conditions, such as psoriasis, eczema, or drug reactions, as well as those with compromised immune systems or a history of systemic illnesses. Both conditions pose increased risk to older adults and people with chronic skin inflammation, but erythroderma carries a higher risk of systemic complications and requires urgent medical attention.
Complications Associated with Each Condition
Psoriasis complications frequently include psoriatic arthritis, which causes joint inflammation and long-term damage, as well as increased risk of cardiovascular disease and metabolic syndrome due to chronic systemic inflammation. Erythroderma carries life-threatening risks such as fluid loss, electrolyte imbalance, and secondary infections owing to extensive skin barrier disruption. Both conditions require careful management to prevent severe systemic complications and improve patient outcomes.
Treatment Strategies: Psoriasis vs Erythroderma
Psoriasis treatment strategies primarily involve topical corticosteroids, vitamin D analogs, phototherapy, and systemic agents like methotrexate, cyclosporine, or biologics targeting TNF-alpha or IL-17/IL-23 pathways. Erythroderma management requires hospitalization, supportive care with fluid and electrolyte balance, temperature regulation, and systemic corticosteroids or immunosuppressants to control inflammation, often addressing underlying causes such as drug reactions or severe psoriasis flare-ups. Both conditions necessitate careful monitoring and tailored therapy to prevent complications and improve patient outcomes.
Prognosis and Long-Term Management
Psoriasis generally has a chronic but manageable prognosis with long-term treatments including topical therapies, phototherapy, and systemic medications to control flare-ups and prevent complications. Erythroderma, often a severe and potentially life-threatening condition, requires prompt hospitalization and aggressive management to address the underlying cause, stabilize skin barrier function, and prevent systemic complications. Long-term management of erythroderma involves close monitoring for relapse, supportive care, and tailored treatment strategies based on etiology, whereas psoriasis demands ongoing maintenance therapy to minimize disease progression and improve quality of life.
Preventive Measures and Patient Education
Effective preventive measures for psoriasis and erythroderma include maintaining skin hydration, avoiding known triggers like stress, infections, or irritants, and adhering to prescribed treatment regimens to reduce flare-ups. Patient education should emphasize recognizing early signs of exacerbation, the importance of regular dermatological follow-up, and lifestyle modifications such as balanced diet and sun protection to manage symptoms and prevent complications. Empowering patients with knowledge about medication adherence, symptom monitoring, and when to seek immediate medical attention can significantly improve disease outcomes.
Psoriasis Infographic
 libterm.com
libterm.com