Sialorrhea and dysphagia are often interconnected conditions that affect saliva control and swallowing function, impacting daily comfort and nutrition. Effective management strategies focus on improving muscle coordination and reducing excessive saliva production to enhance quality of life. Explore the full article to understand the causes, symptoms, and treatments available for these challenging disorders.
Table of Comparison
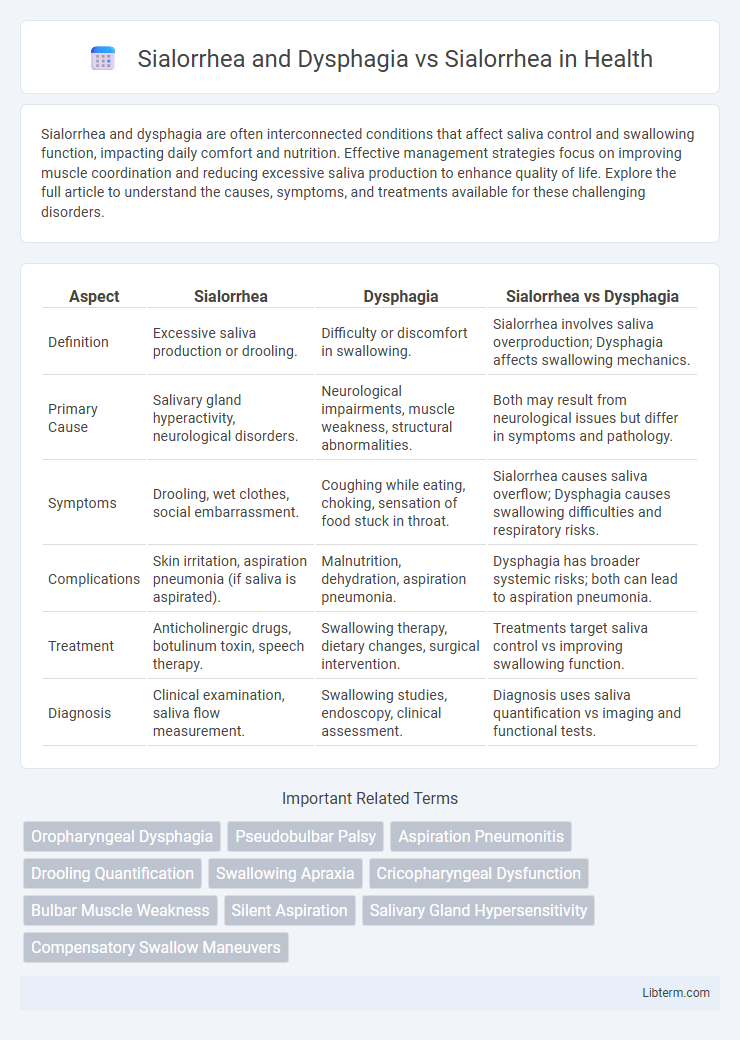
| Aspect | Sialorrhea | Dysphagia | Sialorrhea vs Dysphagia |
|---|---|---|---|
| Definition | Excessive saliva production or drooling. | Difficulty or discomfort in swallowing. | Sialorrhea involves saliva overproduction; Dysphagia affects swallowing mechanics. |
| Primary Cause | Salivary gland hyperactivity, neurological disorders. | Neurological impairments, muscle weakness, structural abnormalities. | Both may result from neurological issues but differ in symptoms and pathology. |
| Symptoms | Drooling, wet clothes, social embarrassment. | Coughing while eating, choking, sensation of food stuck in throat. | Sialorrhea causes saliva overflow; Dysphagia causes swallowing difficulties and respiratory risks. |
| Complications | Skin irritation, aspiration pneumonia (if saliva is aspirated). | Malnutrition, dehydration, aspiration pneumonia. | Dysphagia has broader systemic risks; both can lead to aspiration pneumonia. |
| Treatment | Anticholinergic drugs, botulinum toxin, speech therapy. | Swallowing therapy, dietary changes, surgical intervention. | Treatments target saliva control vs improving swallowing function. |
| Diagnosis | Clinical examination, saliva flow measurement. | Swallowing studies, endoscopy, clinical assessment. | Diagnosis uses saliva quantification vs imaging and functional tests. |
Understanding Sialorrhea: Definition and Causes
Sialorrhea, characterized by excessive saliva production or impaired saliva control, often results from neurological disorders, medication side effects, or oral motor dysfunction. Dysphagia involves difficulty swallowing, which can exacerbate sialorrhea by impairing saliva clearance and increasing drooling risk. Understanding sialorrhea's underlying causes, including neurological conditions like Parkinson's disease and stroke, is crucial for accurate diagnosis and effective treatment strategies.
Dysphagia Explained: Symptoms and Underlying Mechanisms
Dysphagia, a swallowing disorder, often coexists with sialorrhea, exacerbating saliva management difficulties. Symptoms of dysphagia include coughing or choking during meals, sensation of food sticking in the throat, and recurrent pneumonia due to aspiration. Underlying mechanisms involve neurological impairments affecting muscle coordination and strength in the oropharyngeal phase of swallowing, leading to ineffective clearance of saliva and food.
Sialorrhea in Isolation: Common Triggers and Risk Factors
Sialorrhea, or excessive saliva production, often occurs independently due to triggers such as oral infections, medication side effects, or neurological disorders like Parkinson's disease. Unlike sialorrhea combined with dysphagia, isolated sialorrhea primarily results from impaired saliva clearance rather than swallowing difficulties. Risk factors for isolated sialorrhea include poor oral muscle control, certain antipsychotic drugs, and conditions that affect autonomic nervous regulation of salivary glands.
The Link Between Sialorrhea and Dysphagia
Sialorrhea, characterized by excessive saliva production or poor saliva control, is frequently linked to dysphagia due to impaired swallowing mechanisms that prevent effective saliva clearance. Dysphagia, a swallowing disorder, exacerbates sialorrhea by causing saliva accumulation in the oral cavity, increasing the risk of aspiration pneumonia. Understanding the neurogenic and muscular pathways involved in both conditions is crucial for developing targeted therapies to manage their overlapping symptoms.
Pathophysiology: How Dysphagia Influences Sialorrhea
Dysphagia contributes to sialorrhea by impairing the coordinated swallowing mechanism, leading to an inability to effectively clear saliva from the oral cavity. Disrupted neural control over the swallowing reflex in conditions like stroke or Parkinson's disease results in saliva accumulation, manifesting as sialorrhea. The pathophysiology involves compromised oropharyngeal muscle function and altered sensory feedback, causing excessive drooling despite normal or increased salivary production.
Clinical Presentation: Differentiating Sialorrhea with and without Dysphagia
Sialorrhea with dysphagia often presents with excessive drooling accompanied by difficulty swallowing, leading to aspiration risk and recurrent respiratory infections. In contrast, sialorrhea without dysphagia primarily manifests as unintentional saliva leakage without significant impairment in swallowing function. Clinical evaluation emphasizes the presence of dysphagia symptoms, such as coughing, choking, and prolonged oral phase, to differentiate the two conditions and guide targeted management strategies.
Diagnostic Approaches for Sialorrhea and Dysphagia
Diagnostic approaches for sialorrhea and dysphagia encompass clinical assessment, including detailed patient history and physical examination focused on swallowing mechanics and salivary flow. Instrumental evaluations such as videofluoroscopic swallowing studies and fiberoptic endoscopic evaluation of swallowing (FEES) are critical for identifying aspiration risks and dysfunctions specific to dysphagia, while sialometry and salivary gland imaging help quantify excessive saliva production in sialorrhea. Combining these targeted diagnostic tools enables precise differentiation and tailored management strategies for patients presenting with overlapping symptoms of sialorrhea and dysphagia.
Management Strategies: Treating Sialorrhea Alone
Management strategies for treating sialorrhea alone primarily involve anticholinergic medications such as glycopyrrolate and scopolamine, which reduce saliva production by inhibiting parasympathetic stimulation. Botulinum toxin injections into salivary glands present a targeted approach that decreases saliva secretion with minimal systemic side effects. Non-pharmacological interventions include behavioral therapies and oral-motor exercises, which aim to improve saliva control without invasive procedures.
Combined Treatment Approaches for Sialorrhea with Dysphagia
Combined treatment approaches for sialorrhea with dysphagia focus on balancing saliva management while ensuring safe swallowing. Botulinum toxin injections into salivary glands reduce saliva production, minimizing drooling without compromising swallowing function. Rehabilitation therapy, including swallowing exercises and postural adjustments, complements pharmacological interventions to optimize patient outcomes and reduce aspiration risk.
Prognosis and Quality of Life: Outcomes for Affected Patients
Sialorrhea combined with dysphagia significantly worsens prognosis compared to sialorrhea alone due to increased risks of aspiration pneumonia and malnutrition, which directly impact morbidity and mortality rates. Quality of life for patients with both conditions is markedly reduced, as dysphagia exacerbates social isolation and anxiety resulting from excessive drooling and swallowing difficulties. Effective management strategies addressing both sialorrhea and dysphagia are essential to improving patient outcomes and overall well-being.
Sialorrhea and Dysphagia Infographic
 libterm.com
libterm.com