Megacolon is a severe condition characterized by an abnormal dilation of the colon, which can sometimes occur as a complication of Crohn's disease, an inflammatory bowel disease causing chronic inflammation of the digestive tract. This dilation can lead to symptoms such as severe abdominal pain, distension, and potentially life-threatening complications if not promptly managed. To understand how these conditions are linked and what treatments may be effective for your health, continue reading the rest of the article.
Table of Comparison
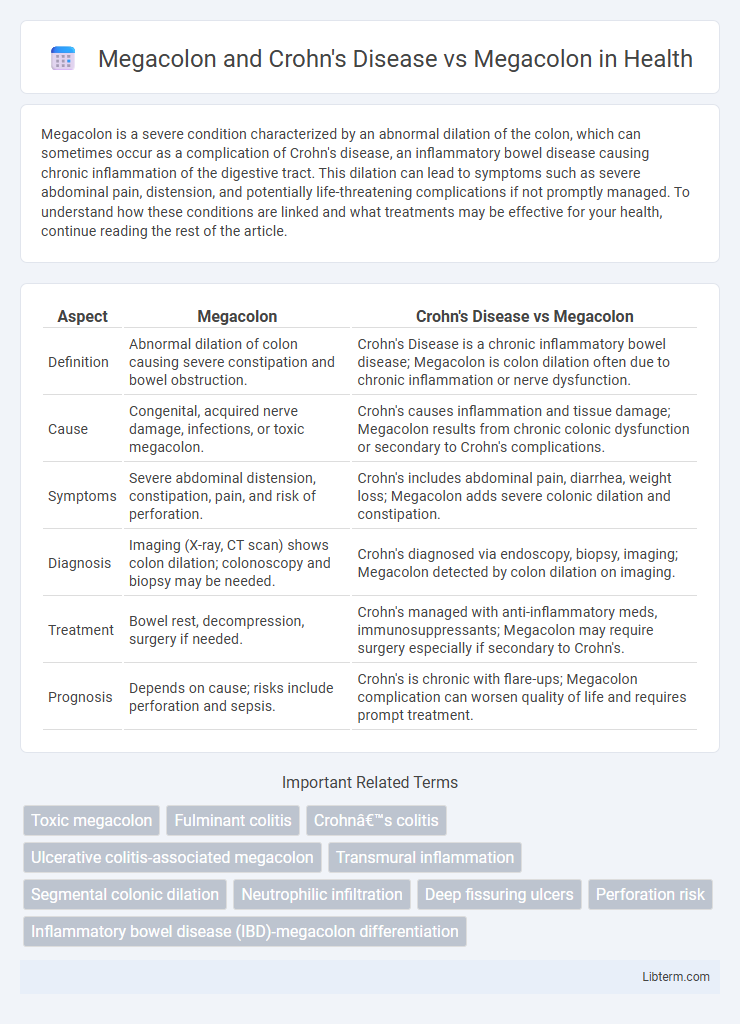
| Aspect | Megacolon | Crohn's Disease vs Megacolon |
|---|---|---|
| Definition | Abnormal dilation of colon causing severe constipation and bowel obstruction. | Crohn's Disease is a chronic inflammatory bowel disease; Megacolon is colon dilation often due to chronic inflammation or nerve dysfunction. |
| Cause | Congenital, acquired nerve damage, infections, or toxic megacolon. | Crohn's causes inflammation and tissue damage; Megacolon results from chronic colonic dysfunction or secondary to Crohn's complications. |
| Symptoms | Severe abdominal distension, constipation, pain, and risk of perforation. | Crohn's includes abdominal pain, diarrhea, weight loss; Megacolon adds severe colonic dilation and constipation. |
| Diagnosis | Imaging (X-ray, CT scan) shows colon dilation; colonoscopy and biopsy may be needed. | Crohn's diagnosed via endoscopy, biopsy, imaging; Megacolon detected by colon dilation on imaging. |
| Treatment | Bowel rest, decompression, surgery if needed. | Crohn's managed with anti-inflammatory meds, immunosuppressants; Megacolon may require surgery especially if secondary to Crohn's. |
| Prognosis | Depends on cause; risks include perforation and sepsis. | Crohn's is chronic with flare-ups; Megacolon complication can worsen quality of life and requires prompt treatment. |
Understanding Megacolon: Definition and Types
Megacolon is characterized by an abnormal dilation of the colon, which can be classified into congenital, acquired, and toxic types based on cause and clinical presentation. In Crohn's disease, megacolon develops primarily due to chronic inflammation leading to bowel wall thickening and motility dysfunction, often resulting in toxic megacolon, a severe, life-threatening complication. Understanding the distinct mechanisms and types of megacolon is crucial for accurate diagnosis and targeted treatment strategies in patients with or without Crohn's disease.
Overview of Crohn’s Disease: Causes and Symptoms
Crohn's Disease is a chronic inflammatory bowel disease characterized by immune system dysregulation leading to inflammation anywhere along the gastrointestinal tract, primarily the terminal ileum and colon. Genetic factors such as NOD2 mutations, environmental triggers, and an abnormal immune response to gut microbiota contribute to disease onset. Common symptoms include abdominal pain, diarrhea, weight loss, and fatigue, often accompanied by complications like strictures and fistulas.
How Crohn’s Disease Relates to Megacolon
Crohn's Disease causes chronic inflammation in the gastrointestinal tract, which can lead to complications such as megacolon due to severe bowel wall damage and impaired motility. Megacolon in Crohn's patients is characterized by abnormal dilation of the colon, often resulting from prolonged inflammation, strictures, or toxic colitis. Unlike idiopathic megacolon, Crohn's-associated megacolon involves underlying autoimmune pathology and requires targeted management addressing the inflammation and structural changes in the bowel.
Key Differences: Megacolon From Crohn’s Disease vs Other Causes
Megacolon from Crohn's disease results from chronic inflammation and transmural bowel wall damage leading to localized or diffuse colonic dilation, whereas megacolon from other causes, such as Hirschsprung's disease or toxic megacolon, often involves neural or muscular dysfunction without primary inflammatory origins. In Crohn's-associated megacolon, strictures, fistulas, and segmental bowel involvement are common pathological features differentiating it from idiopathic or infectious etiologies. Imaging studies typically reveal skip lesions and bowel wall thickening in Crohn's disease, contrasting with uniform dilation or absence of segmental inflammation seen in other megacolon forms.
Clinical Presentation: Signs and Symptoms Compared
Megacolon associated with Crohn's Disease often presents with chronic abdominal pain, diarrhea, weight loss, and intermittent fever, reflecting underlying inflammation and bowel wall thickening. In contrast, idiopathic megacolon typically manifests as severe constipation, abdominal distension, and lack of peristalsis without systemic inflammatory signs. Both conditions may share symptoms like abdominal distension and discomfort, but Crohn's-related megacolon uniquely includes systemic symptoms and inflammatory markers due to autoimmune involvement.
Diagnostic Approaches: Megacolon vs Megacolon in Crohn’s
Diagnostic approaches for megacolon in Crohn's disease primarily involve imaging studies such as abdominal X-rays, CT scans, and MRI to assess colonic dilation alongside inflammation and transmural bowel involvement typical of Crohn's. Contrast studies and colonoscopy with biopsy are essential to differentiate Crohn's-related megacolon from other causes by identifying granulomas, skip lesions, and mucosal ulcerations characteristic of Crohn's disease. In contrast, diagnostic evaluation of idiopathic or toxic megacolon focuses more on clinical presentation combined with imaging and stool studies to rule out infectious etiologies, with less emphasis on mucosal biopsies unless inflammatory bowel disease is suspected.
Complications Associated with Megacolon and Crohn’s Disease
Complications associated with megacolon in Crohn's disease include severe bowel obstruction, perforation, and toxic megacolon, which can lead to life-threatening sepsis and require urgent surgical intervention. Crohn's disease-related inflammation exacerbates colonic wall damage, increasing the risk of abscesses, fistulas, and chronic malabsorption. In contrast, idiopathic megacolon complications primarily involve chronic constipation, abdominal distension, and progressive colonic dilation, often necessitating surgical resection when conservative treatments fail.
Treatment Strategies: Megacolon Alone vs Megacolon with Crohn’s
Treatment strategies for megacolon alone primarily focus on bowel decompression, laxatives, and in severe cases, surgical resection of the affected colon segment. In contrast, megacolon with Crohn's disease requires a more complex approach combining immunosuppressive therapy, biologics to control inflammation, and sometimes surgery to address strictures or perforations while managing megacolon symptoms. Tailoring treatment to the inflammatory component of Crohn's alongside conventional megacolon interventions optimizes clinical outcomes and reduces complications.
Prognosis and Outcome: Comparative Analysis
Megacolon associated with Crohn's Disease often presents a complicated prognosis due to chronic inflammation, which increases the risk of strictures, fistulas, and potential colon perforation, significantly affecting patient outcomes. In contrast, idiopathic or toxic megacolon, unrelated to Crohn's, can result in acute colonic dilation with rapid progression and potentially fatal outcomes if not promptly treated; however, surgical intervention frequently improves prognosis. Comparative outcome data indicate that Crohn's-related megacolon typically requires long-term management and monitoring to prevent relapse, whereas non-Crohn's megacolon cases may have a more immediate but potentially resolvable clinical course.
Preventive Measures and Long-Term Management
Preventive measures for megacolon, especially in the context of Crohn's Disease, emphasize regular monitoring of bowel function and early intervention with anti-inflammatory medications to reduce intestinal inflammation and prevent colonic dilation. Long-term management includes a combination of dietary modifications, immunosuppressive therapies, and, in severe cases, surgical options such as colectomy to address complications and maintain bowel health. Close collaboration with gastroenterologists ensures tailored treatment plans that minimize the risk of megacolon development and improve quality of life for patients with Crohn's Disease.
Megacolon and Crohn's Disease Infographic
 libterm.com
libterm.com