Tenosynovitis is the inflammation of the sheath surrounding a tendon, leading to pain, swelling, and restricted movement. It commonly affects areas such as the wrists, hands, and feet, often caused by repetitive strain or infection. Discover effective treatments and prevention strategies in the following article to help you manage this condition.
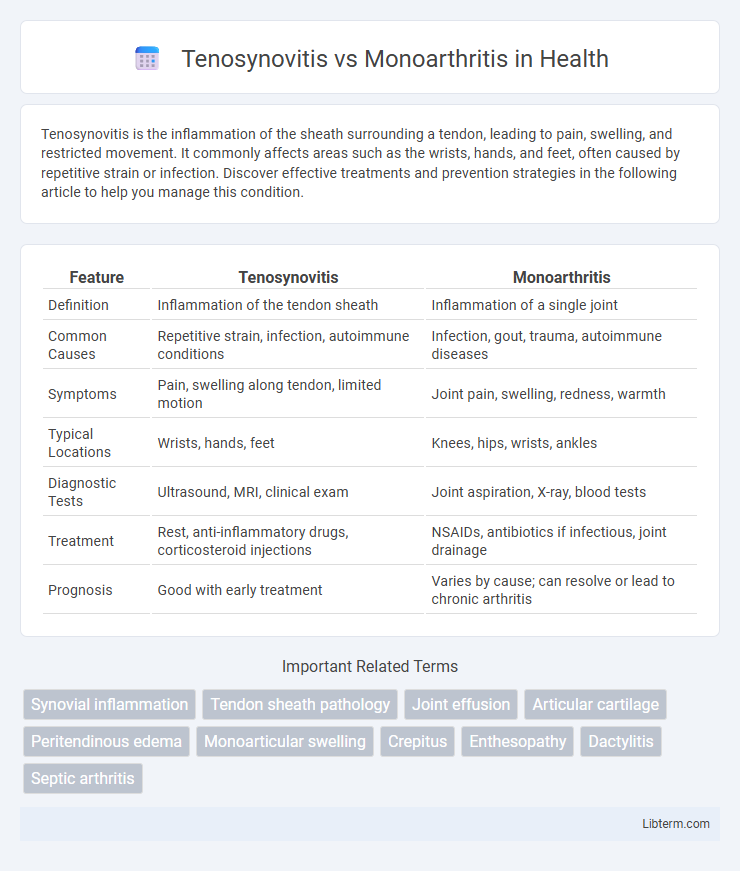
Table of Comparison
| Feature | Tenosynovitis | Monoarthritis |
|---|---|---|
| Definition | Inflammation of the tendon sheath | Inflammation of a single joint |
| Common Causes | Repetitive strain, infection, autoimmune conditions | Infection, gout, trauma, autoimmune diseases |
| Symptoms | Pain, swelling along tendon, limited motion | Joint pain, swelling, redness, warmth |
| Typical Locations | Wrists, hands, feet | Knees, hips, wrists, ankles |
| Diagnostic Tests | Ultrasound, MRI, clinical exam | Joint aspiration, X-ray, blood tests |
| Treatment | Rest, anti-inflammatory drugs, corticosteroid injections | NSAIDs, antibiotics if infectious, joint drainage |
| Prognosis | Good with early treatment | Varies by cause; can resolve or lead to chronic arthritis |
Overview of Tenosynovitis and Monoarthritis
Tenosynovitis is the inflammation of the synovial sheath surrounding a tendon, often caused by repetitive motion, infection, or autoimmune conditions, leading to pain and restricted movement. Monoarthritis refers to inflammation affecting a single joint, commonly due to trauma, infection, or crystal-induced arthritis such as gout. Differentiating between tenosynovitis and monoarthritis involves clinical evaluation and imaging, with tenosynovitis showing tendon sheath swelling while monoarthritis presents as joint effusion and synovial inflammation.
Key Differences Between Tenosynovitis and Monoarthritis
Tenosynovitis primarily involves inflammation of the tendon sheath, leading to pain and restricted movement along tendons, while monoarthritis affects a single joint with inflammation, swelling, and stiffness. Clinical examination reveals tenosynovitis through tendon tenderness and crepitus, whereas monoarthritis presents with joint effusion and warmth localized to the affected joint. Diagnostic imaging like ultrasound shows fluid-filled tendon sheaths in tenosynovitis, contrasting with joint space narrowing and synovial thickening in monoarthritis cases.
Common Causes and Risk Factors
Tenosynovitis commonly results from repetitive strain injuries, autoimmune diseases like rheumatoid arthritis, or infections, affecting the tendon sheath. Monoarthritis primarily arises from gout, septic arthritis, or trauma, leading to inflammation in a single joint. Risk factors for tenosynovitis include repetitive motions and systemic inflammatory conditions, while monoarthritis risk factors involve metabolic disorders, joint injuries, and bacterial infections.
Clinical Presentation and Symptoms
Tenosynovitis primarily presents with localized pain, swelling, and tenderness along the tendon sheath, often accompanied by reduced range of motion and a characteristic crepitus during movement. Monoarthritis typically manifests as acute joint inflammation with severe pain, swelling, warmth, and limited mobility in a single joint, frequently involving the knee, hip, or wrist. Both conditions can cause joint stiffness, but tenosynovitis pain worsens with tendon movement while monoarthritis pain intensifies with joint loading and activity.
Diagnostic Approaches and Imaging Techniques
Tenosynovitis diagnosis primarily relies on clinical examination supported by ultrasound imaging, which effectively visualizes tendon sheath inflammation and fluid accumulation. Monoarthritis evaluation involves synovial fluid analysis obtained via joint aspiration alongside imaging modalities like X-ray and MRI to detect joint space narrowing, effusion, or bone erosions. MRI provides detailed soft tissue contrast crucial for distinguishing tenosynovitis from intra-articular pathologies commonly seen in monoarthritis.
Laboratory Findings in Tenosynovitis vs Monoarthritis
Laboratory findings in tenosynovitis often reveal mild or no inflammatory markers elevation, with normal or slightly increased erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), reflecting localized tendon sheath inflammation. In contrast, monoarthritis typically shows significant elevation of inflammatory markers, including high ESR and CRP levels, and synovial fluid analysis may reveal increased leukocytes, crystals, or microbial pathogens indicative of infection or crystal-induced arthritis. Synovial fluid cultures and serological tests are crucial for differentiating infectious tenosynovitis from septic monoarthritis, guiding appropriate clinical management.
Treatment Strategies for Each Condition
Treatment strategies for tenosynovitis primarily involve anti-inflammatory medications such as NSAIDs, corticosteroid injections, and immobilization of the affected tendon sheath to reduce pain and swelling. In contrast, monoarthritis treatment targets the underlying cause, including antibiotics for infectious arthritis, urate-lowering therapy for gout, or disease-modifying antirheumatic drugs (DMARDs) for autoimmune etiologies. Physical therapy plays a vital role in both conditions to restore joint function and prevent stiffness.
Prognosis and Potential Complications
Tenosynovitis prognosis is generally favorable with early anti-inflammatory treatment, but delayed care can lead to tendon rupture or chronic pain. Monoarthritis often requires identifying the underlying cause, such as infection or crystal deposition, to prevent joint destruction and persistent disability. Both conditions risk long-term joint dysfunction if not promptly and effectively managed.
Preventive Measures and Patient Education
Effective preventive measures for tenosynovitis include maintaining proper ergonomics during repetitive activities, frequent breaks to reduce tendon strain, and early intervention with anti-inflammatory treatments to avoid chronic inflammation. For monoarthritis, prevention focuses on managing underlying conditions like gout or infections through diet control, medication adherence, and prompt treatment of joint injuries to reduce flare-ups. Patient education emphasizes recognizing early symptoms, adhering to prescribed therapies, and adopting lifestyle changes tailored to the specific condition to minimize joint damage and improve long-term outcomes.
When to Refer to a Specialist
Referral to a specialist is warranted in cases of tenosynovitis when symptoms persist beyond two weeks despite initial treatment, or if there is suspicion of infectious or inflammatory causes requiring advanced diagnostic evaluation. Monoarthritis referral is critical when joint swelling and pain are acute, unexplained, or associated with systemic symptoms such as fever, indicating possible septic arthritis or crystal-induced arthritis that necessitate prompt specialist intervention. Early specialist involvement ensures accurate diagnosis and prevents complications in both conditions.
Tenosynovitis Infographic
 libterm.com
libterm.com