Pancreatitis is a serious inflammation of the pancreas that can cause severe abdominal pain and digestive issues. Early diagnosis and treatment are crucial to prevent complications like infection, chronic damage, or organ failure. Discover more about symptoms, causes, and effective management strategies in the rest of this article.
Table of Comparison
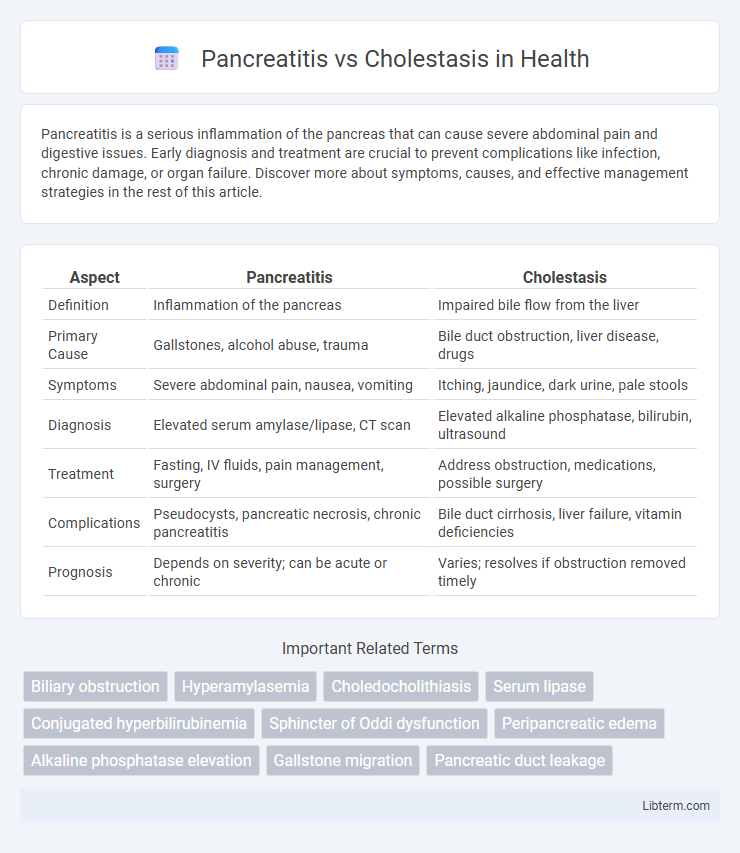
| Aspect | Pancreatitis | Cholestasis |
|---|---|---|
| Definition | Inflammation of the pancreas | Impaired bile flow from the liver |
| Primary Cause | Gallstones, alcohol abuse, trauma | Bile duct obstruction, liver disease, drugs |
| Symptoms | Severe abdominal pain, nausea, vomiting | Itching, jaundice, dark urine, pale stools |
| Diagnosis | Elevated serum amylase/lipase, CT scan | Elevated alkaline phosphatase, bilirubin, ultrasound |
| Treatment | Fasting, IV fluids, pain management, surgery | Address obstruction, medications, possible surgery |
| Complications | Pseudocysts, pancreatic necrosis, chronic pancreatitis | Bile duct cirrhosis, liver failure, vitamin deficiencies |
| Prognosis | Depends on severity; can be acute or chronic | Varies; resolves if obstruction removed timely |
Understanding Pancreatitis and Cholestasis
Pancreatitis is the inflammation of the pancreas causing severe abdominal pain, digestive enzyme disruption, and potential organ damage, often triggered by gallstones or chronic alcohol use. Cholestasis involves impaired bile flow from the liver, leading to bile buildup, jaundice, and itching, commonly resulting from bile duct obstruction or liver diseases. Understanding these conditions requires recognizing the distinct pathophysiological mechanisms: pancreatic enzyme activation in pancreatitis versus bile secretion impairment in cholestasis.
Causes of Pancreatitis vs Cholestasis
Pancreatitis is primarily caused by gallstones blocking the pancreatic duct or excessive alcohol consumption triggering pancreatic inflammation. Cholestasis results from impaired bile flow due to bile duct obstruction, liver diseases such as primary biliary cirrhosis, or certain medications. Understanding these distinct etiologies is crucial for accurate diagnosis and targeted treatment strategies.
Key Symptoms: Pancreatitis vs Cholestasis
Pancreatitis primarily presents with severe upper abdominal pain radiating to the back, nausea, vomiting, and elevated pancreatic enzymes such as amylase and lipase. Cholestasis is characterized by jaundice, pruritus, dark urine, pale stools, and elevated bilirubin and alkaline phosphatase levels. Differentiating key symptoms and laboratory markers is essential for accurate diagnosis and treatment of pancreatitis versus cholestasis.
Diagnostic Approaches for Both Conditions
Pancreatitis diagnosis relies on elevated serum amylase and lipase levels, abdominal ultrasound, and contrast-enhanced CT scans to assess pancreatic inflammation and complications. Cholestasis diagnosis involves liver function tests showing elevated alkaline phosphatase and gamma-glutamyl transferase, along with imaging modalities like MRCP and ultrasound to detect bile duct obstruction or intrahepatic cholestasis. Both conditions benefit from targeted imaging and laboratory tests to differentiate pancreatic inflammation from bile flow impairment effectively.
Laboratory Marker Differences
Pancreatitis is typically characterized by elevated serum amylase and lipase levels, with lipase being more specific and sensitive for diagnosis. Cholestasis often presents with increased alkaline phosphatase (ALP), gamma-glutamyl transferase (GGT), and bilirubin levels, reflecting bile duct obstruction or impaired bile flow. Unlike pancreatitis, cholestasis shows minimal or no elevation in pancreatic enzymes but marked increases in cholestatic liver enzymes and conjugated bilirubin.
Imaging Techniques for Accurate Diagnosis
Imaging techniques for diagnosing pancreatitis primarily include abdominal ultrasound, contrast-enhanced CT scan, and MRI/MRCP, which effectively identify pancreatic inflammation, necrosis, and fluid collections. In contrast, cholestasis diagnosis relies heavily on ultrasound to detect bile duct dilation and gallstones, with MRCP and ERCP providing detailed visualization of biliary obstruction. Precise imaging differentiation is essential for targeted treatment, as pancreatitis shows pancreatic tissue changes while cholestasis involves bile duct abnormalities.
Treatment Options: Pancreatitis Compared to Cholestasis
Treatment options for pancreatitis primarily involve fasting to rest the pancreas, intravenous fluids to maintain hydration, and pain management, with severe cases potentially requiring surgery or endoscopic interventions. Cholestasis treatment focuses on addressing the underlying cause such as bile duct obstruction or liver diseases, using medications like ursodeoxycholic acid to improve bile flow and alleviate symptoms. Both conditions may require nutritional support and close monitoring, but pancreatitis demands more aggressive interventions to prevent complications, whereas cholestasis management targets bile production and flow restoration.
Potential Complications of Each Condition
Pancreatitis can lead to severe complications such as pancreatic necrosis, pseudocyst formation, and systemic inflammatory response syndrome (SIRS), increasing the risk of organ failure. Cholestasis may result in bile duct obstruction, leading to jaundice, fat-soluble vitamin deficiencies, and secondary biliary cirrhosis if untreated. Both conditions pose risks of infection and chronic damage, necessitating prompt diagnosis and management to prevent long-term morbidity.
Prognosis and Recovery Outlook
Pancreatitis prognosis varies widely depending on severity, with mild cases often resolving within weeks and severe cases leading to complications like necrosis or organ failure, negatively impacting recovery. Cholestasis, particularly when chronic, can cause progressive liver damage, increasing the risk of cirrhosis and requiring long-term management for bile flow restoration. Recovery outlook for pancreatitis hinges on early intervention and avoidance of triggers, whereas cholestasis prognosis depends on underlying cause treatment and bile duct functionality maintenance.
Preventive Measures and Risk Reduction
Preventive measures for pancreatitis include maintaining a low-fat diet, avoiding excessive alcohol consumption, and managing underlying conditions like gallstones and hypertriglyceridemia to reduce inflammation of the pancreas. Cholestasis prevention focuses on avoiding hepatotoxic substances, controlling bile duct obstructions, and managing liver diseases such as hepatitis or cirrhosis to ensure proper bile flow. Regular health screenings and lifestyle modifications can significantly reduce risks associated with both pancreatitis and cholestasis.
Pancreatitis Infographic
 libterm.com
libterm.com