Cyanosis is a medical condition characterized by a bluish discoloration of the skin and mucous membranes, indicating low oxygen levels in the blood. It can signal serious underlying issues such as respiratory or cardiovascular problems that require prompt evaluation and treatment. Discover more about the causes, symptoms, and effective management of cyanosis by reading the full article.
Table of Comparison
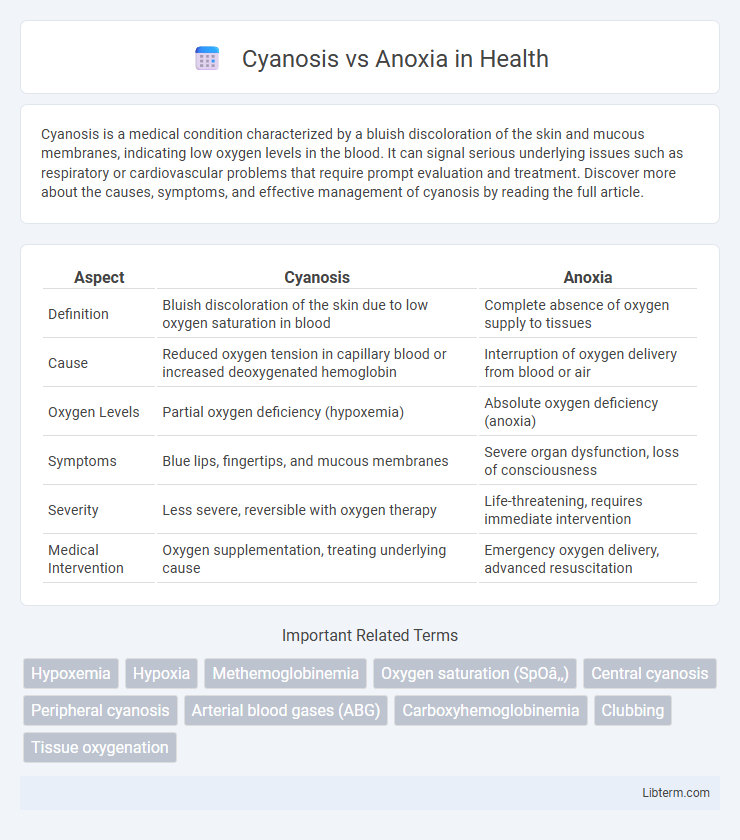
| Aspect | Cyanosis | Anoxia |
|---|---|---|
| Definition | Bluish discoloration of the skin due to low oxygen saturation in blood | Complete absence of oxygen supply to tissues |
| Cause | Reduced oxygen tension in capillary blood or increased deoxygenated hemoglobin | Interruption of oxygen delivery from blood or air |
| Oxygen Levels | Partial oxygen deficiency (hypoxemia) | Absolute oxygen deficiency (anoxia) |
| Symptoms | Blue lips, fingertips, and mucous membranes | Severe organ dysfunction, loss of consciousness |
| Severity | Less severe, reversible with oxygen therapy | Life-threatening, requires immediate intervention |
| Medical Intervention | Oxygen supplementation, treating underlying cause | Emergency oxygen delivery, advanced resuscitation |
Understanding Cyanosis: Definition and Causes
Cyanosis is a clinical condition characterized by a bluish discoloration of the skin and mucous membranes caused by low oxygen saturation in the blood, typically below 85%. It results from increased levels of deoxygenated hemoglobin, often due to respiratory or circulatory disorders such as chronic obstructive pulmonary disease (COPD), congenital heart defects, or pulmonary embolism. Understanding cyanosis involves recognizing its different forms--central cyanosis indicating systemic oxygen deprivation and peripheral cyanosis suggesting localized blood flow issues.
An Overview of Anoxia: Meaning and Etiology
Anoxia refers to the complete absence of oxygen supply to tissues, resulting in severe cellular damage and impaired organ function. Common etiologies include respiratory arrest, severe anemia, carbon monoxide poisoning, and vascular obstructions causing deprivation of oxygen at the cellular level. Unlike cyanosis, which is a bluish discoloration due to deoxygenated hemoglobin, anoxia directly indicates total oxygen deficiency, often leading to critical hypoxic injury.
Key Differences Between Cyanosis and Anoxia
Cyanosis is characterized by a bluish discoloration of the skin and mucous membranes due to inadequate oxygenation of hemoglobin in the blood, whereas anoxia refers to a complete lack of oxygen supply to tissues. Cyanosis typically indicates low arterial oxygen saturation levels, often above 85%, while anoxia results in cellular dysfunction and tissue damage due to total oxygen deprivation. The clinical presentation of cyanosis is visible externally, while anoxia is primarily diagnosed through biochemical markers and neurological symptoms.
Clinical Signs and Symptoms
Cyanosis presents as a bluish discoloration of the skin, lips, and nail beds, indicating insufficient oxygen saturation in the blood, often accompanied by respiratory distress, tachypnea, and cold extremities. Anoxia, characterized by a complete lack of oxygen supply to tissues, leads to rapid neurological impairment, loss of consciousness, and potential organ failure without necessarily showing skin discoloration. Clinical differentiation relies on the presence of hypoxic signs in cyanosis versus the severe systemic effects and altered mental status seen in anoxia.
Underlying Pathophysiology
Cyanosis results from increased deoxygenated hemoglobin in the blood, typically caused by impaired oxygen delivery or abnormal hemoglobin function, leading to a bluish discoloration of the skin and mucous membranes. Anoxia is characterized by a complete absence of oxygen supply to tissues, causing cellular hypoxia and potential tissue death due to the failure of oxidative phosphorylation in mitochondria. Both conditions disrupt normal oxygen transport but differ in severity and the extent of tissue oxygen deprivation.
Diagnostic Methods and Tools
Diagnostic methods for cyanosis primarily include pulse oximetry, arterial blood gas (ABG) analysis, and co-oximetry to assess oxygen saturation levels and differentiate between central and peripheral cyanosis. In contrast, anoxia diagnosis relies heavily on ABG analysis to measure partial pressure of oxygen (PaO2) and tissue oxygenation studies such as near-infrared spectroscopy (NIRS) to evaluate cellular oxygen deprivation. Imaging techniques like chest X-rays or echocardiography support identifying underlying causes in both conditions, enhancing diagnostic accuracy.
Risk Factors and Associated Conditions
Cyanosis commonly results from conditions causing inadequate oxygenation of hemoglobin, such as chronic obstructive pulmonary disease (COPD), congenital heart defects, and pulmonary embolism, with risk factors including tobacco smoking and structural lung or heart abnormalities. Anoxia arises from severe oxygen deprivation at the tissue level, often linked to conditions like cardiac arrest, severe anemia, carbon monoxide poisoning, and stroke, with risk factors involving asphyxiation, high-altitude exposure, and vascular obstruction. Both conditions require prompt diagnosis and management due to their association with critical impairments in oxygen delivery and potential organ damage.
Treatment Approaches for Cyanosis
Treatment approaches for cyanosis primarily target the underlying cause of reduced oxygenation or impaired blood flow. Administering supplemental oxygen is common to increase arterial oxygen saturation, while addressing conditions such as congenital heart defects, respiratory infections, or pulmonary embolism may require specific medical interventions or surgery. In severe cases, advanced therapies like mechanical ventilation or extracorporeal membrane oxygenation (ECMO) might be necessary to restore adequate tissue oxygenation.
Management Strategies for Anoxia
Management strategies for anoxia prioritize rapid restoration of oxygen delivery to tissues through supplemental oxygen therapy and advanced airway management, including intubation if necessary. Continuous monitoring of blood oxygen saturation via pulse oximetry and arterial blood gases guides treatment adjustments, while addressing underlying causes such as cardiac or respiratory failure is essential. In severe cases, hyperbaric oxygen therapy and use of vasopressors to maintain tissue perfusion serve as critical interventions to prevent irreversible cellular damage.
Prognosis and Long-term Outcomes
Cyanosis commonly indicates inadequate oxygenation but often allows for reversible conditions with timely intervention, generally resulting in a favorable prognosis. Anoxia, reflecting complete oxygen deprivation to tissues, typically leads to severe cellular injury and poorer long-term outcomes, including neurological deficits or organ failure. Early diagnosis and prompt treatment significantly influence recovery and minimize long-term complications in both conditions.
Cyanosis Infographic
 libterm.com
libterm.com