Atrial fibrillation is a common heart rhythm disorder characterized by rapid and irregular beating of the atria, increasing the risk of stroke and heart failure. Managing this condition involves lifestyle changes, medication, and sometimes medical procedures to restore normal heart rhythm. Discover more about symptoms, treatment options, and prevention strategies in the rest of the article.
Table of Comparison
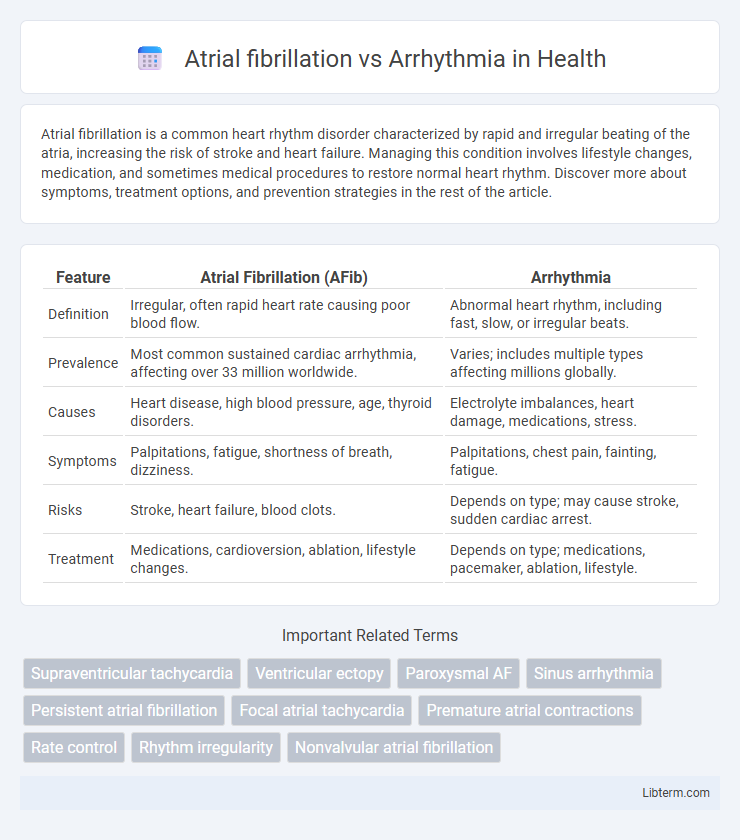
| Feature | Atrial Fibrillation (AFib) | Arrhythmia |
|---|---|---|
| Definition | Irregular, often rapid heart rate causing poor blood flow. | Abnormal heart rhythm, including fast, slow, or irregular beats. |
| Prevalence | Most common sustained cardiac arrhythmia, affecting over 33 million worldwide. | Varies; includes multiple types affecting millions globally. |
| Causes | Heart disease, high blood pressure, age, thyroid disorders. | Electrolyte imbalances, heart damage, medications, stress. |
| Symptoms | Palpitations, fatigue, shortness of breath, dizziness. | Palpitations, chest pain, fainting, fatigue. |
| Risks | Stroke, heart failure, blood clots. | Depends on type; may cause stroke, sudden cardiac arrest. |
| Treatment | Medications, cardioversion, ablation, lifestyle changes. | Depends on type; medications, pacemaker, ablation, lifestyle. |
Introduction to Cardiac Rhythm Disorders
Atrial fibrillation is a specific type of arrhythmia characterized by rapid and irregular heartbeats originating in the atria, leading to impaired blood flow and increased stroke risk. Arrhythmia refers broadly to any abnormal heart rhythm, encompassing a variety of conditions including bradycardia, tachycardia, and atrial fibrillation itself. Understanding cardiac rhythm disorders involves recognizing these irregularities' impact on cardiac function and the potential complications arising from impaired electrical signal conduction within the heart.
Defining Arrhythmia: Types and Classifications
Arrhythmia refers to any irregularity in the heart's rhythm, including variations in heartbeat speed or pattern, and encompasses a broad range of classified types such as tachycardia, bradycardia, and fibrillation. Atrial fibrillation is a specific type of arrhythmia characterized by rapid, irregular beating of the atria, leading to inefficient blood flow and increased risk of stroke. Classifying arrhythmias involves analyzing the origin of abnormal rhythms--supraventricular versus ventricular--and their impact on heart function, aiding in targeted treatment strategies.
Understanding Atrial Fibrillation: Causes and Risk Factors
Atrial fibrillation is a specific type of arrhythmia characterized by irregular and often rapid heart rhythm originating in the atria, leading to inefficient blood flow. Key causes include high blood pressure, coronary artery disease, and structural heart abnormalities, while risk factors encompass age, obesity, diabetes, and excessive alcohol consumption. Understanding these elements is crucial for distinguishing atrial fibrillation from other arrhythmias and guiding effective treatment strategies.
Key Differences between Atrial Fibrillation and Other Arrhythmias
Atrial fibrillation is characterized by rapid, irregular electrical signals in the atria, leading to an erratic heartbeat, whereas other arrhythmias may involve abnormal rhythms originating from the ventricles or involve slower heart rates. Unlike atrial fibrillation, which increases the risk of stroke due to blood pooling and clot formation in the atria, some arrhythmias like bradycardia cause abnormally slow heartbeats that can reduce oxygen delivery. Treatment approaches differ as atrial fibrillation often requires anticoagulants and rate control medications, while other arrhythmias may be managed with pacemakers or ablation depending on their type and origin.
Symptoms: How AFib and Arrhythmias Present Clinically
Atrial fibrillation (AFib) often presents with palpitations, irregular heartbeat, fatigue, and shortness of breath, whereas general arrhythmias can range from benign skipped beats to severe symptoms like dizziness, chest pain, or syncope depending on the type. AFib typically causes an irregularly irregular pulse and may lead to stroke risk due to atrial thrombus formation. Clinical presentation varies widely, but the hallmark of AFib is rapid, disorganized atrial electrical activity, distinct from other arrhythmias that may involve bradycardia or tachycardia with different electrocardiographic patterns.
Diagnostic Approaches for AFib vs Arrhythmias
Diagnostic approaches for atrial fibrillation (AFib) primarily involve electrocardiograms (ECG) to detect irregular heart rhythms and Holter monitors for continuous cardiac rhythm tracking over 24-48 hours. In contrast, arrhythmias require a wider range of diagnostic tools, including event recorders for intermittent symptoms, electrophysiological studies for detailed mapping, and cardiac imaging to assess structural abnormalities. Biomarkers and wearable cardiac devices have become increasingly important in differentiating AFib from other types of arrhythmias and tailoring patient-specific management.
Treatment Strategies: AFib Compared to General Arrhythmias
Treatment strategies for atrial fibrillation (AFib) primarily focus on rate control, rhythm control, and anticoagulation to prevent stroke, with medications like beta-blockers, antiarrhythmics, and anticoagulants being cornerstone therapies. General arrhythmias encompass a wider range of abnormal heart rhythms, requiring tailored treatments such as catheter ablation, implantable devices, or lifestyle modifications depending on the specific type and severity. AFib treatment often emphasizes managing thromboembolic risk, whereas general arrhythmia management varies widely based on the arrhythmia's origin and cardiac impact.
Complications and Prognosis of AFib vs Other Arrhythmias
Atrial fibrillation (AFib) significantly increases the risk of ischemic stroke, heart failure, and systemic embolism compared to other arrhythmias, due to its irregular atrial contractions leading to blood stasis and thrombus formation. Prognosis in AFib patients often involves higher morbidity and mortality rates, with a need for long-term anticoagulation therapy to prevent stroke, while some other arrhythmias, such as benign premature atrial contractions, typically carry a lower risk of serious complications. Early diagnosis and appropriate management strategies are critical to improving outcomes and reducing complications associated with AFib versus other arrhythmias.
Preventive Measures and Lifestyle Modifications
Atrial fibrillation and other arrhythmias demand targeted preventive measures such as blood pressure control, weight management, and reduction of alcohol and caffeine intake to minimize the risk of onset and complications. Regular physical activity, stress reduction techniques, and avoiding tobacco use are critical lifestyle modifications shown to improve heart rhythm stability and overall cardiovascular health. Monitoring underlying conditions like hypertension, diabetes, and sleep apnea plays a vital role in preventing arrhythmia progression and atrial fibrillation episodes.
Frequently Asked Questions: AFib and Arrhythmia Differences
Atrial fibrillation (AFib) is a specific type of arrhythmia characterized by rapid and irregular beating of the atria, while arrhythmia refers to any irregularity in the heart's rhythm, including bradycardia and tachycardia. Frequently asked questions highlight that AFib increases the risk of stroke and heart failure more significantly than other arrhythmias. Understanding these differences is crucial for proper diagnosis and treatment planning.
Atrial fibrillation Infographic
 libterm.com
libterm.com