Atopic dermatitis is a chronic skin condition characterized by inflammation, redness, and intense itching that can significantly impact your quality of life. Effective management involves maintaining proper skin hydration, avoiding irritants, and using prescribed treatments to reduce flare-ups. Discover practical tips and expert advice in the rest of this article to better control your symptoms and improve your skin health.
Table of Comparison
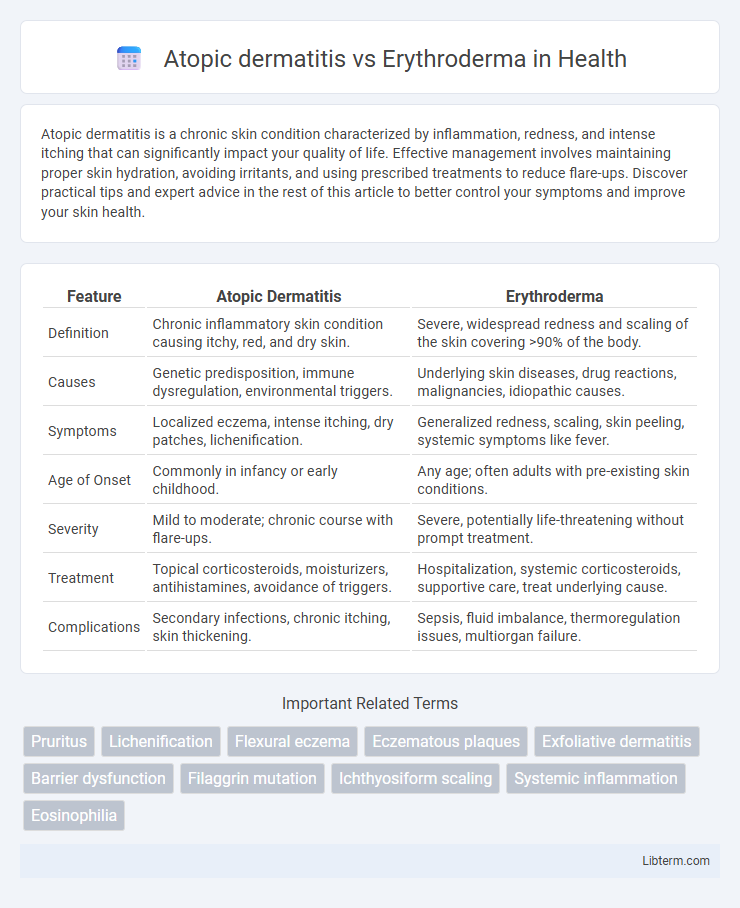
| Feature | Atopic Dermatitis | Erythroderma |
|---|---|---|
| Definition | Chronic inflammatory skin condition causing itchy, red, and dry skin. | Severe, widespread redness and scaling of the skin covering >90% of the body. |
| Causes | Genetic predisposition, immune dysregulation, environmental triggers. | Underlying skin diseases, drug reactions, malignancies, idiopathic causes. |
| Symptoms | Localized eczema, intense itching, dry patches, lichenification. | Generalized redness, scaling, skin peeling, systemic symptoms like fever. |
| Age of Onset | Commonly in infancy or early childhood. | Any age; often adults with pre-existing skin conditions. |
| Severity | Mild to moderate; chronic course with flare-ups. | Severe, potentially life-threatening without prompt treatment. |
| Treatment | Topical corticosteroids, moisturizers, antihistamines, avoidance of triggers. | Hospitalization, systemic corticosteroids, supportive care, treat underlying cause. |
| Complications | Secondary infections, chronic itching, skin thickening. | Sepsis, fluid imbalance, thermoregulation issues, multiorgan failure. |
Introduction to Atopic Dermatitis and Erythroderma
Atopic dermatitis is a chronic inflammatory skin condition characterized by itchy, red, and dry skin, commonly affecting children and adults with a history of allergies or asthma. Erythroderma, also known as exfoliative dermatitis, involves widespread redness and scaling covering more than 90% of the body surface, often resulting from underlying skin diseases or systemic conditions. Both conditions require accurate diagnosis and tailored treatment approaches due to their differing etiologies and clinical presentations.
Definition and Overview
Atopic dermatitis is a chronic inflammatory skin condition characterized by itchy, red, and dry patches, primarily caused by genetic and environmental factors that disrupt the skin barrier and immune response. Erythroderma, also known as exfoliative dermatitis, involves widespread redness and scaling covering more than 90% of the body surface, often resulting from severe underlying dermatologic diseases, drug reactions, or systemic conditions. Both conditions exhibit significant inflammation but differ in extent, severity, and underlying causes, making accurate diagnosis critical for effective management.
Epidemiology and Prevalence
Atopic dermatitis affects 15-20% of children and 1-3% of adults worldwide, with higher prevalence in urban and developed regions. Erythroderma, a rare and severe dermatological condition, has an incidence of approximately 1 in 100,000 individuals, often linked to underlying diseases such as psoriasis or drug reactions. Both conditions display distinct epidemiological patterns, with atopic dermatitis exhibiting early onset and erythroderma occurring primarily in adults across diverse populations.
Etiology and Risk Factors
Atopic dermatitis arises primarily from genetic predisposition involving filaggrin gene mutations, leading to skin barrier dysfunction, whereas erythroderma results from diverse causes including drug reactions, underlying malignancies, or pre-existing dermatoses. Risk factors for atopic dermatitis include family history of allergies or asthma and environmental triggers such as allergens and irritants. In contrast, erythroderma risk factors encompass extensive skin involvement from psoriasis, cutaneous T-cell lymphoma, or adverse drug reactions, requiring prompt identification to prevent systemic complications.
Clinical Presentation and Symptoms
Atopic dermatitis commonly presents with intense itching, dry, scaly, and erythematous plaques primarily localized to flexural areas such as the elbows and knees, accompanied by a chronic relapsing course. Erythroderma manifests as widespread erythema and exfoliation involving over 90% of the body surface, often accompanied by systemic symptoms like fever and malaise. While atopic dermatitis involves localized inflammation and pruritus, erythroderma represents a severe, generalized inflammatory skin condition requiring urgent evaluation due to its potential systemic complications.
Pathophysiology and Mechanisms
Atopic dermatitis involves a complex interplay of genetic predisposition, epidermal barrier dysfunction, and immune dysregulation, primarily characterized by a Th2-skewed immune response leading to chronic inflammation and increased IgE production. Erythroderma, a severe inflammatory condition, results from widespread skin inflammation causing extensive epidermal exfoliation and altered cytokine profiles, often triggered by underlying dermatoses, drug reactions, or malignancies. Both conditions involve immune system alterations and barrier impairment, but erythroderma represents a life-threatening systemic response with more pronounced epidermal disruption and immune activation than the localized chronic inflammation typical of atopic dermatitis.
Diagnostic Criteria and Differential Diagnosis
Atopic dermatitis is diagnosed based on chronic or relapsing eczematous lesions, intense pruritus, and typical distribution patterns such as flexural areas, supported by a personal or family history of atopy. Erythroderma is characterized by widespread erythema and scaling covering more than 90% of the body surface, often associated with systemic symptoms and requires evaluation of underlying causes such as drug reactions, psoriasis, or malignancies. Differential diagnosis involves distinguishing atopic dermatitis from erythroderma by assessing lesion extent, associated systemic features, and histopathological findings to guide appropriate management.
Treatment Approaches and Management Strategies
Atopic dermatitis treatment emphasizes moisturizing, topical corticosteroids, and calcineurin inhibitors to reduce inflammation and prevent flare-ups, often complemented by antihistamines for itching control. Erythroderma management requires identifying and treating the underlying cause, intensive systemic therapy including systemic corticosteroids or immunosuppressants, and supportive care to maintain fluid balance and prevent infections. Both conditions benefit from patient education and avoiding triggers, but erythroderma demands vigilant medical supervision due to its potential severity and systemic complications.
Prognosis and Long-term Outcomes
Atopic dermatitis generally has a chronic but manageable course with appropriate treatment, rarely leading to severe complications, whereas erythroderma carries a more serious prognosis due to widespread skin involvement and potential systemic complications such as infection, fluid imbalance, and organ failure. Long-term outcomes for atopic dermatitis often involve intermittent flare-ups with periods of remission, while erythroderma may result in prolonged hospitalization and requires urgent diagnosis to address underlying causes like drug reactions or malignancies. Effective management strategies for erythroderma are critical to improving survival rates and minimizing permanent skin damage, contrasting with the typically favorable outlook seen in well-controlled atopic dermatitis.
Key Differences Between Atopic Dermatitis and Erythroderma
Atopic dermatitis is a chronic inflammatory skin condition characterized by itchy, red, and dry patches, primarily affecting children and adults with a history of allergies or asthma. Erythroderma, also known as exfoliative dermatitis, is a severe and widespread redness and scaling of the skin that can arise from underlying conditions like psoriasis, drug reactions, or atopic dermatitis itself. Key differences include the extent and severity of skin involvement, with atopic dermatitis typically presenting localized lesions, whereas erythroderma involves more than 90% of the body surface area and may lead to systemic symptoms such as fever and lymphadenopathy.
Atopic dermatitis Infographic
 libterm.com
libterm.com