Thrombocytosis is a medical condition characterized by an abnormally high number of platelets in the blood, which can increase the risk of clotting or bleeding complications. Causes range from reactive responses to infections or inflammation, to bone marrow disorders requiring careful diagnosis. Discover more about the symptoms, risks, and treatment options to manage your health effectively in the full article.
Table of Comparison
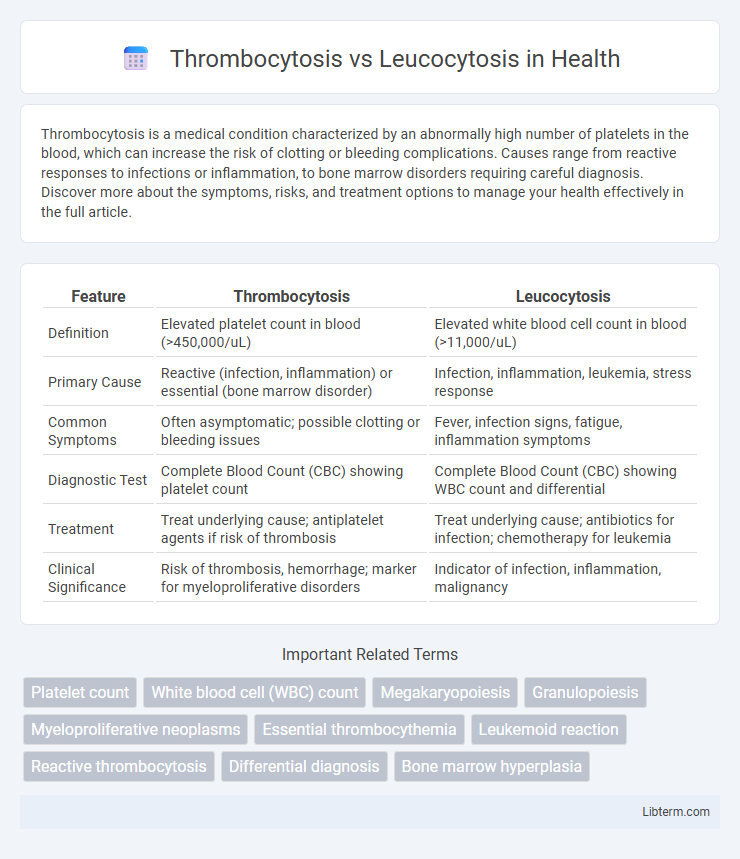
| Feature | Thrombocytosis | Leucocytosis |
|---|---|---|
| Definition | Elevated platelet count in blood (>450,000/uL) | Elevated white blood cell count in blood (>11,000/uL) |
| Primary Cause | Reactive (infection, inflammation) or essential (bone marrow disorder) | Infection, inflammation, leukemia, stress response |
| Common Symptoms | Often asymptomatic; possible clotting or bleeding issues | Fever, infection signs, fatigue, inflammation symptoms |
| Diagnostic Test | Complete Blood Count (CBC) showing platelet count | Complete Blood Count (CBC) showing WBC count and differential |
| Treatment | Treat underlying cause; antiplatelet agents if risk of thrombosis | Treat underlying cause; antibiotics for infection; chemotherapy for leukemia |
| Clinical Significance | Risk of thrombosis, hemorrhage; marker for myeloproliferative disorders | Indicator of infection, inflammation, malignancy |
Introduction to Thrombocytosis and Leucocytosis
Thrombocytosis refers to an abnormally high platelet count in the blood, often exceeding 450,000 platelets per microliter, which can increase the risk of clotting disorders. Leucocytosis denotes an elevated white blood cell (WBC) count, typically above 11,000 cells per microliter, indicating an immune response to infections, inflammation, or hematologic diseases. Both conditions serve as important clinical markers guiding diagnosis and treatment in hematology and internal medicine.
Overview of Blood Cell Types
Thrombocytosis is characterized by an elevated platelet count, which plays a crucial role in blood clotting and wound healing, while leucocytosis involves an increased white blood cell count that is essential for immune defense and fighting infections. Platelets are small, anucleate cell fragments derived from megakaryocytes, whereas white blood cells comprise various types such as neutrophils, lymphocytes, monocytes, eosinophils, and basophils, each with distinct immune functions. Understanding the differences in these blood cell types is vital for diagnosing and managing conditions related to abnormal cell proliferation or immune responses.
Definition of Thrombocytosis
Thrombocytosis is a medical condition characterized by an abnormally high platelet count in the blood, typically exceeding 450,000 platelets per microliter, which can increase the risk of thrombosis or blood clots. In contrast, leucocytosis refers to an elevated white blood cell count, often indicating infection or inflammation. Thrombocytosis may be classified as primary, caused by bone marrow disorders like essential thrombocythemia, or secondary, as a reactive response to conditions such as infection, inflammation, or iron deficiency.
Definition of Leucocytosis
Leucocytosis is defined as an elevated white blood cell (WBC) count above the normal range, often exceeding 11,000 cells per microliter in adults. This condition typically indicates an immune response to infections, inflammation, stress, or hematologic malignancies such as leukemia. Unlike thrombocytosis, which involves an increase in platelet count, leucocytosis specifically pertains to white blood cells and serves as a critical marker for diagnosing and monitoring various pathological states.
Causes of Thrombocytosis
Thrombocytosis is primarily caused by reactive conditions such as infections, inflammation, iron deficiency, or tissue damage, while essential thrombocythemia represents a myeloproliferative disorder leading to excessive platelet production. In contrast, leucocytosis is mainly driven by infections, stress responses, leukemia, or autoimmune diseases, manifesting as elevated white blood cell counts. Understanding the underlying causes of thrombocytosis is crucial for accurate diagnosis and appropriate management.
Causes of Leucocytosis
Leucocytosis primarily results from infections, inflammation, stress, trauma, or hematologic malignancies such as leukemia. It reflects an increased white blood cell count as the immune system responds to these pathological or physiological stimuli. Unlike thrombocytosis, which involves elevated platelet levels often due to bone marrow disorders or reactive causes, leucocytosis specifically signals an immune response or malignancy.
Clinical Manifestations: Thrombocytosis vs Leucocytosis
Thrombocytosis commonly presents with symptoms such as headache, dizziness, visual disturbances, and increased risk of thrombosis or bleeding due to abnormal platelet function. Leucocytosis often manifests with signs of infection or inflammation, including fever, chills, malaise, and localized symptoms depending on the underlying cause, such as respiratory distress or urinary discomfort. Differentiating clinical features include thrombotic events in thrombocytosis versus infectious or inflammatory signs in leucocytosis.
Diagnostic Approaches and Laboratory Findings
Thrombocytosis diagnosis involves complete blood count (CBC) revealing elevated platelet counts above 450,000/uL, often confirmed by bone marrow biopsy to assess megakaryocyte proliferation. Leucocytosis diagnosis requires CBC showing increased white blood cell (WBC) counts exceeding 11,000/uL, with differentiation between neutrophilia or lymphocytosis guiding further tests such as blood smears or flow cytometry. Laboratory findings for thrombocytosis include reactive causes like inflammation or iron deficiency and primary causes such as essential thrombocythemia, while leucocytosis often indicates infections, leukemias, or inflammatory diseases distinguished by specific WBC subtype elevations.
Treatment Options for Thrombocytosis and Leucocytosis
Treatment options for thrombocytosis primarily involve antiplatelet agents like aspirin to reduce the risk of clotting, cytoreductive therapy such as hydroxyurea for high-risk patients, and addressing underlying causes like inflammation or iron deficiency. Leucocytosis treatment targets the root cause, for example, antibiotics for infections or chemotherapy for leukemia-related elevation, with supportive care like hydration and monitoring for complications. Both conditions require tailored approaches based on severity, symptoms, and underlying etiologies to optimize patient outcomes.
Key Differences and Clinical Significance
Thrombocytosis refers to an elevated platelet count above 450,000/uL, commonly linked to reactive causes like inflammation or primary myeloproliferative disorders such as essential thrombocythemia, whereas leucocytosis indicates an increased white blood cell count typically exceeding 11,000/uL, often signaling infection, inflammation, or hematologic malignancies like leukemia. Clinically, thrombocytosis raises risks of thrombosis and bleeding complications, necessitating platelet function evaluation, while leucocytosis guides infection management and diagnostic workup for marrow or immune dysregulation. Differentiating these conditions impacts treatment strategies, including cytoreductive therapy for thrombocytosis or antibiotics and immunomodulation for leucocytosis.
Thrombocytosis Infographic
 libterm.com
libterm.com