Viremia occurs when viruses circulate in the bloodstream, allowing them to spread rapidly throughout the body and infect multiple organs. Detecting viremia is crucial for diagnosing viral infections and assessing their severity. Explore the rest of this article to understand how viremia impacts your health and its management strategies.
Table of Comparison
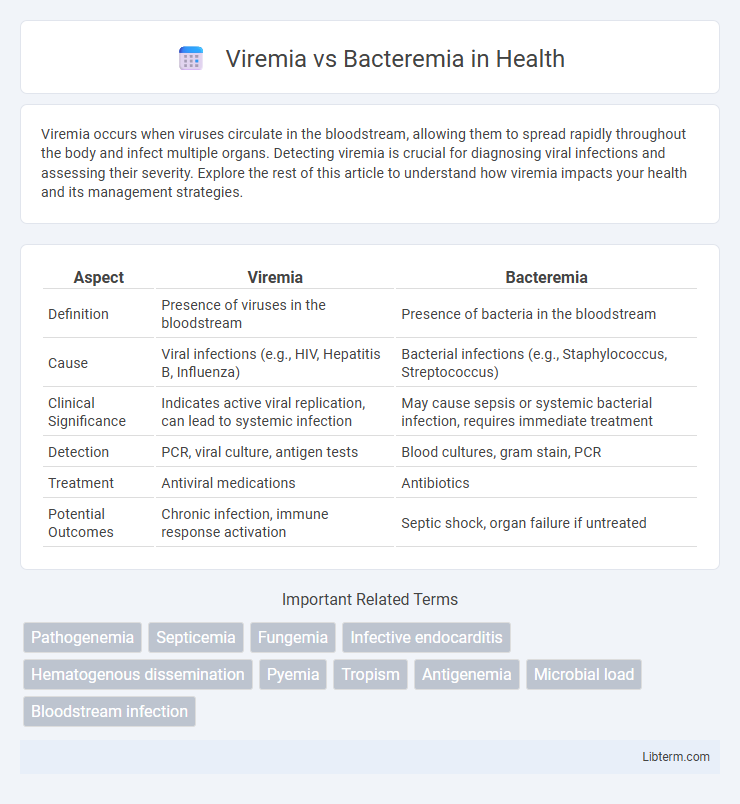
| Aspect | Viremia | Bacteremia |
|---|---|---|
| Definition | Presence of viruses in the bloodstream | Presence of bacteria in the bloodstream |
| Cause | Viral infections (e.g., HIV, Hepatitis B, Influenza) | Bacterial infections (e.g., Staphylococcus, Streptococcus) |
| Clinical Significance | Indicates active viral replication, can lead to systemic infection | May cause sepsis or systemic bacterial infection, requires immediate treatment |
| Detection | PCR, viral culture, antigen tests | Blood cultures, gram stain, PCR |
| Treatment | Antiviral medications | Antibiotics |
| Potential Outcomes | Chronic infection, immune response activation | Septic shock, organ failure if untreated |
Introduction to Viremia and Bacteremia
Viremia refers to the presence of viruses in the bloodstream, often indicating an active viral infection that can spread to multiple organs. Bacteremia is characterized by the presence of bacteria in the blood, which may result from infections such as pneumonia, urinary tract infections, or surgical procedures. Both conditions are critical to diagnose early, as they can lead to systemic infections like sepsis if untreated.
Definitions and Core Differences
Viremia refers to the presence of viruses in the bloodstream, whereas bacteremia indicates the presence of bacteria in the blood. Viremia often results from viral infections like HIV or hepatitis, and can be transient or persistent, affecting viral load and disease progression. Bacteremia can lead to serious conditions such as sepsis if bacteria multiply and spread, with bloodstream infections often diagnosed through blood cultures to identify the specific bacterial pathogens.
Causes and Sources of Infection
Viremia occurs when viruses enter the bloodstream, commonly originating from respiratory infections, gastrointestinal viruses, or systemic viral diseases such as influenza, HIV, or hepatitis. Bacteremia involves the presence of bacteria in the blood, often resulting from infections like dental procedures, urinary tract infections, or invasive surgeries that introduce pathogens such as Staphylococcus aureus or Escherichia coli. Both conditions arise from different infectious sources, with viremia linked to viral replication and dissemination, while bacteremia stems from bacterial invasion secondary to localized infection or medical interventions.
Pathogenesis: Viral vs. Bacterial Spread in Blood
Viremia involves the presence of viruses in the bloodstream, facilitating the systemic spread of viral particles through infected host cells or free virions, whereas bacteremia refers to bacteria circulating in blood, often resulting from localized infections or invasive procedures. Viral pathogenesis in viremia depends on the ability of viruses to infect and replicate within host cells, leading to cell lysis and dissemination, while bacterial pathogenesis in bacteremia typically involves evasion of the immune system, adhesion to endothelial cells, and potential formation of biofilms. The immune response differs significantly, with viremia triggering antiviral cytokines and bacteremia often provoking a robust inflammatory response aimed at bacterial clearance.
Clinical Manifestations and Symptoms
Viremia, characterized by the presence of viruses in the bloodstream, often presents with systemic symptoms such as fever, fatigue, muscle aches, and malaise due to viral replication and immune response activation. Bacteremia involves bacteria circulating in the blood and can cause clinical manifestations ranging from mild fever and chills to severe sepsis, characterized by hypotension, organ dysfunction, and septic shock in advanced cases. Both conditions may present with overlapping signs like fever and malaise, but bacteremia frequently leads to more pronounced inflammatory responses and septic complications.
Diagnostic Approaches and Laboratory Findings
Viremia is detected through molecular techniques like PCR and viral culture, which identify viral nucleic acids or particles in blood samples, whereas bacteremia diagnosis relies on blood cultures to isolate and identify bacterial pathogens. Laboratory findings in viremia typically reveal viral load quantification alongside serological markers such as IgM and IgG antibodies, while bacteremia is indicated by positive blood cultures, elevated white blood cell counts, and markers of systemic inflammation like C-reactive protein and procalcitonin. Accurate differentiation between viremia and bacteremia is critical for guiding targeted antimicrobial or antiviral therapy and improving patient outcomes.
Complications and Health Risks
Viremia, the presence of viruses in the bloodstream, can lead to severe complications such as systemic viral infections, immune system hyperactivation, and potential organ damage including myocarditis or encephalitis. Bacteremia, defined by bacteria circulating in the blood, poses a risk for sepsis, septic shock, and metastatic infections like endocarditis or osteomyelitis. Both conditions demand prompt medical intervention to prevent progression to life-threatening systemic inflammatory response syndrome (SIRS) and multi-organ failure.
Treatment Strategies for Viremia and Bacteremia
Treatment strategies for viremia primarily involve antiviral medications such as nucleoside analogs, protease inhibitors, and interferons to suppress viral replication and enhance immune response. Bacteremia requires prompt administration of targeted antibiotics based on culture sensitivity to eliminate the bacterial pathogen and prevent sepsis or systemic complications. Supportive care, including intravenous fluids and monitoring for organ dysfunction, is critical in managing severe cases of both viremia and bacteremia to improve patient outcomes.
Prevention Methods and Risk Reduction
Effective prevention methods for viremia emphasize vaccination, maintaining proper hygiene, and avoiding exposure to infected individuals or contaminated fluids. Preventing bacteremia involves strict adherence to sterile techniques during medical procedures, timely treatment of infections, and managing chronic conditions such as diabetes. Both conditions require prompt identification and targeted interventions to reduce the risk of systemic spread and serious complications.
Prognosis and Outcomes
Viremia typically results in transient infections with generally self-limiting outcomes, although persistent viremia can lead to chronic diseases or systemic complications depending on the virus type. Bacteremia poses a higher risk of severe prognosis, often progressing to sepsis or septic shock if untreated, significantly increasing morbidity and mortality rates. Early detection and appropriate antimicrobial therapy are crucial in bacteremia to improve patient outcomes, whereas antiviral management depends on the specific viral pathogen involved.
Viremia Infographic
 libterm.com
libterm.com