Eosinopenia is a condition characterized by an abnormally low number of eosinophils in the blood, often signaling acute infections, stress, or the use of corticosteroids. This decrease in eosinophils can impact your immune system's ability to respond to allergens and parasitic infections effectively. Discover more about the causes, symptoms, and treatment options for eosinopenia in the rest of this article.
Table of Comparison
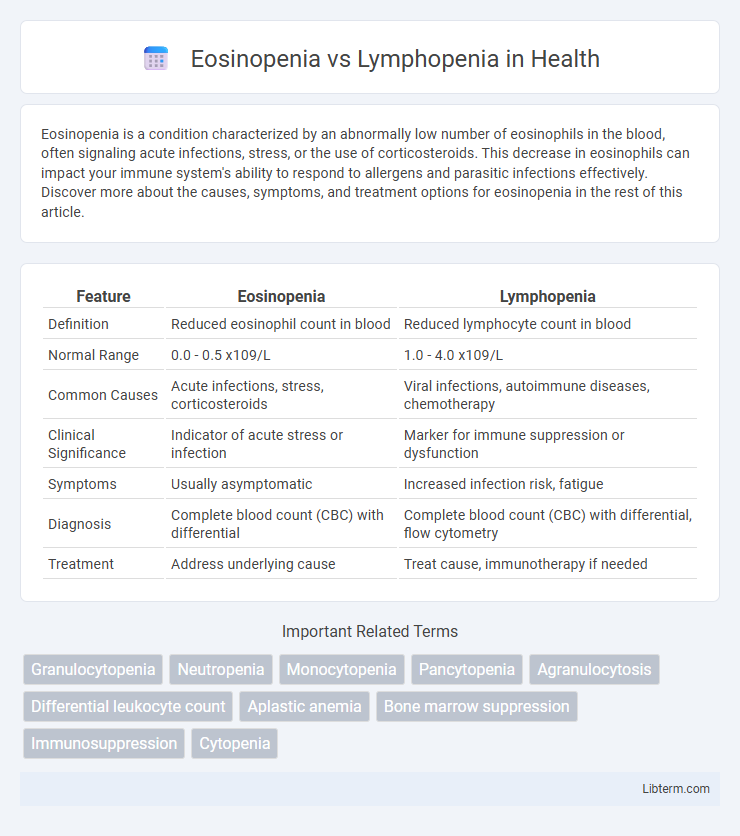
| Feature | Eosinopenia | Lymphopenia |
|---|---|---|
| Definition | Reduced eosinophil count in blood | Reduced lymphocyte count in blood |
| Normal Range | 0.0 - 0.5 x109/L | 1.0 - 4.0 x109/L |
| Common Causes | Acute infections, stress, corticosteroids | Viral infections, autoimmune diseases, chemotherapy |
| Clinical Significance | Indicator of acute stress or infection | Marker for immune suppression or dysfunction |
| Symptoms | Usually asymptomatic | Increased infection risk, fatigue |
| Diagnosis | Complete blood count (CBC) with differential | Complete blood count (CBC) with differential, flow cytometry |
| Treatment | Address underlying cause | Treat cause, immunotherapy if needed |
Introduction to Eosinopenia and Lymphopenia
Eosinopenia refers to an abnormally low count of eosinophils, a type of white blood cell involved in allergic reactions and parasitic infections, often linked to acute stress or corticosteroid use. Lymphopenia, also known as lymphocytopenia, indicates a reduced number of lymphocytes, critical for adaptive immunity and fighting viral infections, commonly associated with immunodeficiency, autoimmune disorders, or chemotherapy. Both conditions serve as important hematologic markers in diagnosing underlying diseases and monitoring immune system status.
Understanding Eosinophils and Lymphocytes
Eosinopenia refers to a lower-than-normal count of eosinophils, a type of white blood cell involved in immune responses against parasites and allergic reactions, while lymphopenia indicates a reduced number of lymphocytes, critical cells responsible for adaptive immunity and viral defense. Eosinophils are granulated leukocytes that play a role in modulating inflammation and combating multicellular parasites, whereas lymphocytes consist mainly of T cells and B cells that orchestrate specific immune responses and antibody production. Differentiating between eosinopenia and lymphopenia is essential for diagnosing conditions like infections, autoimmune disorders, and hematologic diseases, as each reflects distinct immune system dysfunctions.
Causes of Eosinopenia
Eosinopenia, characterized by a decreased eosinophil count, is primarily caused by acute stress responses such as corticosteroid therapy, severe infections, and Cushing's syndrome, which suppress eosinophil production or promote their redistribution. In contrast, lymphopenia involves a reduction in lymphocytes and is often linked to viral infections, immunodeficiency disorders, or chemotherapy. Understanding the distinct etiologies of eosinopenia is crucial for differentiating it from lymphopenia in clinical practice.
Causes of Lymphopenia
Lymphopenia, characterized by a decreased lymphocyte count, primarily results from viral infections such as HIV, autoimmune diseases like lupus, malnutrition, or immunosuppressive therapies including chemotherapy and corticosteroids. In contrast, eosinopenia represents a low eosinophil count often linked to acute infections, stress response, or corticosteroid use. Understanding lymphopenia's etiology is crucial for diagnosing immune deficiencies and monitoring patient immune status during treatment.
Clinical Manifestations: Eosinopenia vs Lymphopenia
Eosinopenia typically presents with reduced eosinophil counts often linked to acute infections, stress response, or corticosteroid use, manifesting clinically as subdued allergic reactions or inflammation. Lymphopenia is characterized by diminished lymphocyte levels, commonly associated with viral infections, immunodeficiency disorders, or chemotherapy, leading to increased susceptibility to infections and impaired immune response. Both conditions impact immune regulation but differ in their clinical manifestations based on the affected cell type and underlying causes.
Diagnostic Approaches and Laboratory Findings
Eosinopenia, characterized by a reduced eosinophil count often below 0.05 x 10^9/L, is typically evaluated through complete blood count (CBC) and is associated with acute stress, infections, or corticosteroid therapy, showing distinct suppression of eosinophils in laboratory findings. Lymphopenia, marked by lymphocyte counts below 1.0 x 10^9/L, is diagnosed by flow cytometry or CBC and linked to viral infections, immunodeficiency, or autoimmune conditions, revealing a reduction in total lymphocyte subsets such as T cells, B cells, and NK cells. Diagnostic differentiation relies on specific leukocyte profiling and clinical correlation, with eosinopenia commonly indicating systemic stress or inflammatory response, while lymphopenia suggests immune compromise or chronic disease.
Common Diseases Associated with Eosinopenia
Eosinopenia, characterized by a decreased eosinophil count, is commonly associated with acute infections, corticosteroid therapy, and stress-related conditions such as sepsis and Cushing's syndrome. In contrast, lymphopenia often occurs in viral infections, HIV/AIDS, autoimmune diseases, and chemotherapy-induced immunosuppression. Understanding the distinct clinical contexts of eosinopenia versus lymphopenia aids in accurate diagnosis and targeted treatment strategies.
Common Diseases Associated with Lymphopenia
Lymphopenia, characterized by a decreased lymphocyte count, is commonly associated with diseases such as HIV/AIDS, tuberculosis, and various autoimmune disorders including lupus and rheumatoid arthritis. Viral infections like influenza and severe acute respiratory syndrome (SARS) also frequently result in lymphopenia due to the depletion of lymphocytes. In contrast, eosinopenia, which involves a reduced eosinophil count, is often linked to acute bacterial infections, corticosteroid therapy, and conditions of physiological stress rather than chronic immune dysfunction.
Prognostic Implications and Treatment Strategies
Eosinopenia and lymphopenia serve as distinct hematologic markers with differing prognostic implications; eosinopenia often indicates acute stress or infection and may correlate with disease severity, while lymphopenia is frequently associated with immunosuppression and poorer outcomes in viral infections and cancers. Treatment strategies for eosinopenia primarily target the underlying cause, such as managing infection or inflammation, whereas lymphopenia requires addressing immune restoration through interventions like immunostimulants, antiviral therapy, or minimizing immunosuppressive agents. Monitoring these conditions aids in guiding clinical decisions, optimizing patient management, and improving prognosis by tailoring therapies to the specific immune dysregulation present.
Key Differences and Clinical Significance
Eosinopenia is characterized by a reduced eosinophil count, often linked to acute stress, infections, or corticosteroid use, while lymphopenia denotes a low lymphocyte count typically associated with viral infections, immunodeficiency, or bone marrow disorders. Clinically, eosinopenia serves as a marker for systemic inflammation and stress responses, whereas lymphopenia indicates impaired immune function and increased susceptibility to opportunistic infections. Understanding these distinct hematologic patterns aids in diagnosing underlying conditions and tailoring patient management strategies effectively.
Eosinopenia Infographic
 libterm.com
libterm.com