Embolism occurs when a blood clot or other substance blocks a blood vessel, potentially causing severe complications such as stroke, heart attack, or pulmonary embolism. Recognizing the symptoms early and understanding the risk factors can be crucial for timely treatment and prevention. Explore the rest of the article to learn how embolism might affect your health and what steps you can take to minimize the risks.
Table of Comparison
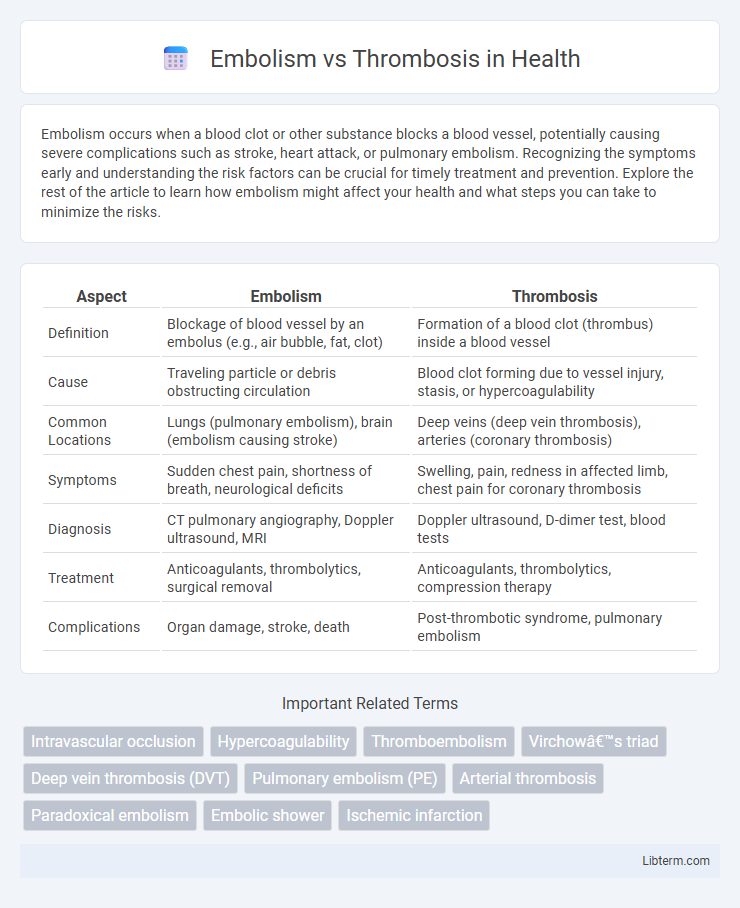
| Aspect | Embolism | Thrombosis |
|---|---|---|
| Definition | Blockage of blood vessel by an embolus (e.g., air bubble, fat, clot) | Formation of a blood clot (thrombus) inside a blood vessel |
| Cause | Traveling particle or debris obstructing circulation | Blood clot forming due to vessel injury, stasis, or hypercoagulability |
| Common Locations | Lungs (pulmonary embolism), brain (embolism causing stroke) | Deep veins (deep vein thrombosis), arteries (coronary thrombosis) |
| Symptoms | Sudden chest pain, shortness of breath, neurological deficits | Swelling, pain, redness in affected limb, chest pain for coronary thrombosis |
| Diagnosis | CT pulmonary angiography, Doppler ultrasound, MRI | Doppler ultrasound, D-dimer test, blood tests |
| Treatment | Anticoagulants, thrombolytics, surgical removal | Anticoagulants, thrombolytics, compression therapy |
| Complications | Organ damage, stroke, death | Post-thrombotic syndrome, pulmonary embolism |
Understanding Embolism and Thrombosis
Embolism occurs when a blood clot, air bubble, fat globule, or other substance travels through the bloodstream and lodges in a vessel, causing a sudden blockage. Thrombosis involves the formation of a blood clot within a blood vessel, impeding normal blood flow at the clot's location. Understanding the distinction between embolism and thrombosis is crucial for accurate diagnosis and effective treatment of vascular disorders.
Key Differences Between Embolism and Thrombosis
Embolism involves the obstruction of a blood vessel by a traveling clot or foreign substance, whereas thrombosis is the formation of a blood clot within a blood vessel at the site of its origin. Emboli can be composed of blood clots, fat, air, or other materials moving through the bloodstream, while thrombosis specifically refers to localized clotting that can restrict or block blood flow. The clinical implications differ as embolism often causes sudden vessel occlusion and ischemia, whereas thrombosis may lead to vessel narrowing, tissue damage, or potentially embolize if fragments dislodge.
Causes of Thrombosis
Thrombosis primarily results from Virchow's triad, which includes endothelial injury, stasis of blood flow, and hypercoagulability. Common causes include prolonged immobility, surgical procedures, malignancies, genetic clotting disorders like Factor V Leiden, and chronic inflammatory conditions. Understanding these factors aids in preventing deep vein thrombosis (DVT) and pulmonary embolism through risk assessment and targeted interventions.
Causes of Embolism
Embolism occurs when a blood clot, fat globule, air bubble, or other material travels through the bloodstream and lodges in a vessel, blocking blood flow. Common causes include deep vein thrombosis, where clots formed in the deep veins dislodge and migrate, and fat embolism syndrome, often triggered by fractures of long bones. Air embolism can result from trauma or medical procedures, while amniotic fluid embolism occurs during labor.
Common Symptoms and Warning Signs
Embolism and thrombosis both involve blood clots that can obstruct blood flow, causing symptoms like sudden pain, swelling, and redness, typically in the limbs. Warning signs of embolism often include sudden shortness of breath, chest pain, or dizziness, indicating a possible pulmonary embolism or stroke. Thrombosis symptoms frequently manifest as localized warmth, tenderness, and discoloration around the affected vein, commonly seen in deep vein thrombosis (DVT).
Diagnostic Approaches for Embolism and Thrombosis
Diagnostic approaches for embolism and thrombosis primarily include imaging techniques such as Doppler ultrasound, which detects blood flow abnormalities and thrombi in veins or arteries. Computed tomography pulmonary angiography (CTPA) is the gold standard for diagnosing pulmonary embolism by visualizing emboli in pulmonary arteries. Laboratory tests like D-dimer assays aid in ruling out thrombotic events, while echocardiography evaluates cardiac sources of emboli and assesses hemodynamic impact.
Treatment Options: Embolism vs Thrombosis
Treatment options for embolism primarily involve anticoagulants such as heparin and warfarin to prevent clot propagation and thrombolytic therapy to dissolve existing clots, while surgical embolectomy may be necessary in severe cases. Thrombosis management includes antiplatelet agents like aspirin and blood thinners to reduce clot formation, coupled with lifestyle modifications to address underlying risk factors such as hypertension and hyperlipidemia. Both conditions require prompt medical intervention tailored to the clot's location and patient's overall health to prevent complications like stroke or pulmonary embolism.
Potential Complications and Risks
Embolism and thrombosis both pose significant risks of vascular obstruction, leading to ischemia and tissue damage. Potential complications of embolism include stroke, pulmonary embolism, and organ infarction depending on the embolus location, while thrombosis primarily risks deep vein thrombosis (DVT), pulmonary embolism, and myocardial infarction. Both conditions increase the likelihood of chronic complications such as post-thrombotic syndrome and long-term vascular insufficiency, necessitating prompt diagnosis and management to prevent morbidity and mortality.
Prevention Strategies for Both Conditions
Prevention strategies for embolism and thrombosis include maintaining a healthy lifestyle with regular exercise, balanced diet, and smoking cessation to reduce risk factors like obesity and hypertension. Anticoagulant medications such as warfarin or direct oral anticoagulants (DOACs) are often prescribed to patients with atrial fibrillation or deep vein thrombosis to prevent clot formation and embolic events. Regular monitoring of blood coagulation levels and managing underlying conditions like diabetes or hyperlipidemia further decrease the likelihood of thromboembolic complications.
Prognosis and Long-Term Management
Prognosis of embolism depends on the size and location of the blockage, with pulmonary embolism carrying a significant risk of mortality if untreated, whereas thrombosis prognosis varies based on the extent of vessel occlusion and underlying conditions. Long-term management for embolism typically involves anticoagulant therapy to prevent recurrence and monitoring for complications such as pulmonary hypertension. In thrombosis, management includes anticoagulation, lifestyle modifications, and regular imaging to assess clot resolution and prevent post-thrombotic syndrome.
Embolism Infographic
 libterm.com
libterm.com