Extradural refers to the space or area located outside the dura mater, the tough outer membrane surrounding the brain and spinal cord. Conditions such as extradural hematomas or abscesses require prompt diagnosis and treatment to prevent serious complications. Explore the rest of the article to understand the causes, symptoms, and management options related to extradural issues.
Table of Comparison
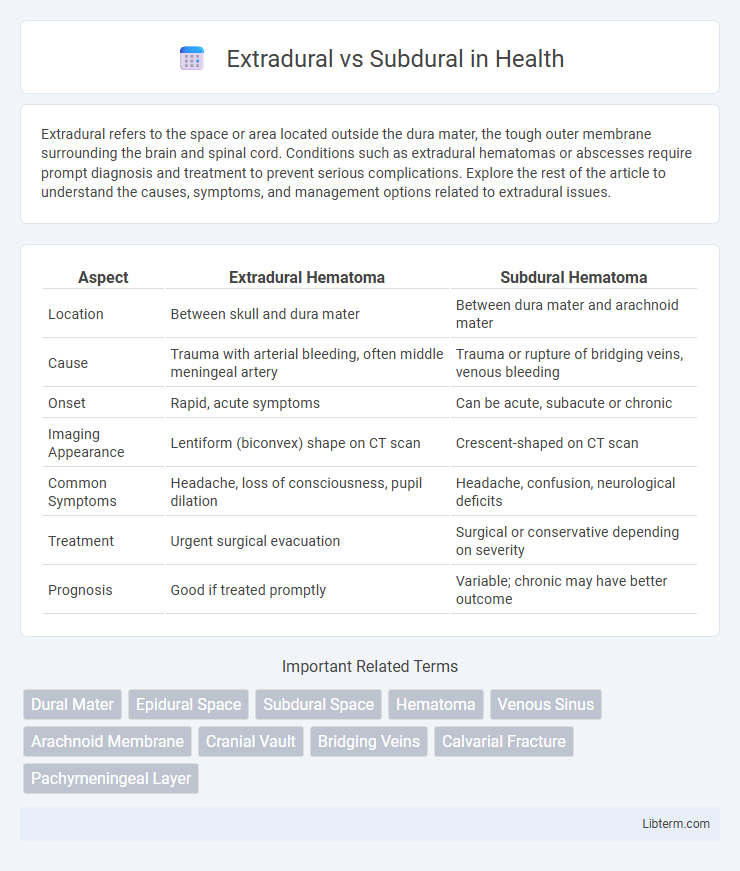
| Aspect | Extradural Hematoma | Subdural Hematoma |
|---|---|---|
| Location | Between skull and dura mater | Between dura mater and arachnoid mater |
| Cause | Trauma with arterial bleeding, often middle meningeal artery | Trauma or rupture of bridging veins, venous bleeding |
| Onset | Rapid, acute symptoms | Can be acute, subacute or chronic |
| Imaging Appearance | Lentiform (biconvex) shape on CT scan | Crescent-shaped on CT scan |
| Common Symptoms | Headache, loss of consciousness, pupil dilation | Headache, confusion, neurological deficits |
| Treatment | Urgent surgical evacuation | Surgical or conservative depending on severity |
| Prognosis | Good if treated promptly | Variable; chronic may have better outcome |
Introduction to Extradural and Subdural Lesions
Extradural lesions occur between the dura mater and the skull, often caused by trauma leading to arterial bleeding, commonly from the middle meningeal artery. Subdural lesions develop between the dura mater and arachnoid mater, typically resulting from venous bleeding due to tearing of bridging veins. Understanding these anatomical differences is crucial for accurate diagnosis and treatment of cranial hematomas.
Anatomical Differences: Extradural vs Subdural Space
The extradural space, also known as the epidural space, lies between the inner surface of the skull and the dura mater, containing fat and blood vessels, primarily the meningeal arteries. In contrast, the subdural space is a potential space located between the dura mater and the arachnoid mater, containing a thin layer of fluid and bridging veins. These anatomical distinctions are critical in diagnosing and managing conditions such as extradural hematomas, which occur above the dura, and subdural hematomas, which occur beneath it.
Causes and Risk Factors
Extradural hematomas typically result from traumatic injury causing damage to the middle meningeal artery, often linked to skull fractures, while subdural hematomas arise from tearing of bridging veins due to rapid head movement or brain atrophy, heightening risk in elderly or anticoagulated patients. Risk factors for extradural hematomas include young age, male gender, and high-impact trauma, whereas subdural hematomas are more common in older adults, chronic alcohol users, and individuals on blood-thinning medications. Both conditions are associated with traumatic brain injury but differ in their vascular origins and patient susceptibility profiles.
Pathophysiology and Mechanisms of Injury
Extradural hematomas occur due to arterial bleeding, typically from the middle meningeal artery, following a temporal bone fracture that causes blood accumulation between the dura mater and the skull, leading to rapid intracranial pressure increase. Subdural hematomas result from venous bleeding caused by tearing of bridging veins between the brain surface and dura mater, often after acceleration-deceleration trauma, causing slower blood pooling beneath the dura. The pathophysiological difference lies in the source of hemorrhage and the space of blood accumulation, influencing clinical presentation and urgency of intervention.
Clinical Presentation and Symptoms
Extradural hematomas typically present with a brief loss of consciousness followed by a lucid interval and rapid neurological deterioration, often accompanied by severe headache, vomiting, and unilateral pupil dilation. Subdural hematomas commonly manifest with gradual onset of symptoms such as headache, confusion, decreased level of consciousness, and focal neurological deficits, particularly in elderly patients or those with a history of trauma. Both conditions require prompt diagnosis through imaging and immediate medical intervention to prevent permanent brain injury.
Diagnostic Imaging: CT and MRI Findings
Extradural hematomas typically appear on CT scans as biconvex, lens-shaped hyperdense collections limited by suture lines, often associated with skull fractures. Subdural hematomas present as crescent-shaped, concave hyperdensities on CT, crossing suture lines but restricted by dural reflections, with acute lesions appearing hyperdense and chronic ones hypodense or isodense. MRI provides superior contrast resolution, where subdural hematomas show variable signal intensity depending on age, and extradural hematomas usually appear as well-defined collections adjacent to the skull, aiding in differentiation and precise localization.
Key Differences in Management Strategies
Extradural hematomas typically require urgent surgical evacuation due to rapid arterial bleeding between the dura mater and the skull, whereas subdural hematomas often involve venous bleeding beneath the dura and may be managed conservatively or surgically based on size and symptoms. Imaging findings on CT scans, such as the lentiform shape in extradural versus the crescent shape in subdural hematomas, guide treatment decisions, with extradural hematomas necessitating faster intervention to prevent brain herniation. Patient age, hematoma chronicity, neurological status, and intracranial pressure monitoring are critical factors influencing the choice between conservative management and craniotomy for subdural hematomas.
Surgical Approaches and Outcomes
Extradural hematomas often require emergent craniotomy or burr hole evacuation to promptly relieve pressure and prevent brain herniation, with surgical outcomes typically favorable if intervention occurs early. Subdural hematomas, especially chronic cases, may be managed with burr hole drainage or craniotomy depending on hematoma size and patient condition, and prognosis varies widely based on patient age, comorbidities, and timing of surgery. Surgical approaches targeting extradural hematomas tend to have lower morbidity due to their epidural location, whereas subdural hematomas involve cortical brain surface, increasing risks of neurological deficits postoperatively.
Prognosis and Complication Rates
Extradural hematomas typically have a better prognosis when treated promptly due to the confined bleeding between the dura mater and the skull, allowing quicker surgical evacuation and lower complication rates. Subdural hematomas, located between the dura and arachnoid membranes, often have a higher risk of complications such as increased intracranial pressure and brain injury, leading to poorer outcomes especially in chronic cases or delayed treatment. The prognosis for subdural hematoma patients is generally less favorable due to the diffuse nature of bleeding and greater likelihood of associated brain damage.
Summary: Extradural vs Subdural at a Glance
Extradural hematomas occur between the skull and dura mater, often caused by arterial injury leading to rapid blood accumulation, while subdural hematomas form between the dura mater and arachnoid layer due to venous bleeding, typically resulting in slower symptom onset. Extradural cases frequently present with a lucid interval followed by rapid neurological decline, whereas subdural hematomas exhibit gradual cognitive impairment and focal neurological deficits. Prompt diagnosis using CT scans differentiates these hematomas, enabling tailored surgical intervention for improved patient outcomes.
Extradural Infographic
 libterm.com
libterm.com