Neutrophilic and eosinophilic inflammation are key indicators in diagnosing various respiratory and allergic conditions, reflecting different immune responses. Understanding the roles of neutrophils and eosinophils can help tailor treatments for diseases like asthma or chronic bronchitis effectively. Explore the rest of the article to learn how these immune cells impact your health and treatment options.
Table of Comparison
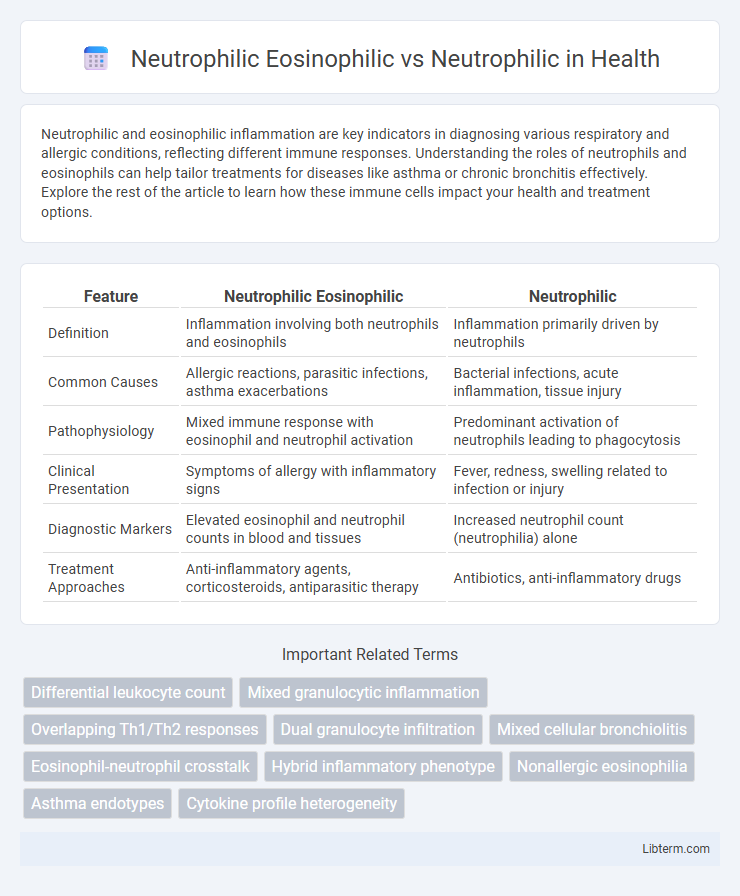
| Feature | Neutrophilic Eosinophilic | Neutrophilic |
|---|---|---|
| Definition | Inflammation involving both neutrophils and eosinophils | Inflammation primarily driven by neutrophils |
| Common Causes | Allergic reactions, parasitic infections, asthma exacerbations | Bacterial infections, acute inflammation, tissue injury |
| Pathophysiology | Mixed immune response with eosinophil and neutrophil activation | Predominant activation of neutrophils leading to phagocytosis |
| Clinical Presentation | Symptoms of allergy with inflammatory signs | Fever, redness, swelling related to infection or injury |
| Diagnostic Markers | Elevated eosinophil and neutrophil counts in blood and tissues | Increased neutrophil count (neutrophilia) alone |
| Treatment Approaches | Anti-inflammatory agents, corticosteroids, antiparasitic therapy | Antibiotics, anti-inflammatory drugs |
Introduction to Neutrophilic and Eosinophilic Inflammation
Neutrophilic inflammation is characterized by the rapid accumulation of neutrophils, the primary immune cells responsible for combating bacterial and fungal infections, and is often associated with acute tissue injury and infection. Eosinophilic inflammation involves the recruitment of eosinophils, which play a crucial role in responses to parasitic infections and allergic reactions, particularly asthma and eosinophilic esophagitis. Understanding the distinct cellular mechanisms and cytokine profiles driving neutrophilic versus eosinophilic inflammation is essential for developing targeted therapies for inflammatory diseases.
Defining Neutrophilic Inflammation
Neutrophilic inflammation is characterized by an increased presence of neutrophils, the primary immune cells responsible for combating bacterial infections and mediating acute inflammatory responses. Neutrophilic-eosinophilic inflammation involves both neutrophils and eosinophils, often reflecting a more complex immune reaction seen in conditions like certain asthma phenotypes, where neutrophils drive tissue damage while eosinophils contribute to allergic or parasitic responses. Understanding the distinct cellular makeup aids in targeted therapeutic strategies, emphasizing the role of neutrophils in acute inflammation versus the combined cellular dynamics in mixed inflammatory states.
Understanding Eosinophilic Inflammation
Eosinophilic inflammation is characterized by the infiltration of eosinophils, a type of white blood cell involved in allergic reactions and parasitic infections, distinguishing it from neutrophilic inflammation which primarily involves neutrophils responsible for responding to bacterial infections. Neutrophilic eosinophilic inflammation denotes a mixed inflammatory response where both neutrophils and eosinophils contribute to tissue damage and disease pathology, commonly observed in conditions such as asthma and chronic rhinosinusitis. Understanding the distinct cellular mechanisms and mediators, including eosinophil-derived cytokines and neutrophil proteases, is critical for developing targeted therapies that address the specific inflammatory profiles.
Neutrophilic Eosinophilic Overlap: What Does It Mean?
Neutrophilic eosinophilic overlap refers to the coexistence of high levels of both neutrophils and eosinophils in the blood or tissues, indicating a complex inflammatory response often seen in respiratory diseases like asthma and chronic obstructive pulmonary disease (COPD). This overlap suggests a mixed inflammatory phenotype that can influence disease severity, treatment response, and progression, requiring tailored therapeutic approaches targeting both cell types. Understanding the neutrophilic eosinophilic overlap helps clinicians optimize management strategies for inflammatory airway conditions, emphasizing personalized medicine.
Mechanisms Driving Neutrophilic Inflammation
Neutrophilic inflammation in both neutrophilic eosinophilic and neutrophilic phenotypes is primarily driven by pro-inflammatory cytokines such as IL-8 and TNF-a, which recruit and activate neutrophils at the site of inflammation. In neutrophilic eosinophilic inflammation, the coexistence of eosinophils amplifies the inflammatory response through the release of eosinophil-derived neurotoxins and cationic proteins that further stimulate neutrophil chemotaxis and activation. The sustained presence of reactive oxygen species (ROS) and proteases from activated neutrophils contributes to tissue damage and chronic inflammation characteristic of neutrophilic-dominant profiles.
Pathophysiology of Neutrophilic Eosinophilic Response
Neutrophilic eosinophilic response involves a synergistic activation of neutrophils and eosinophils, driven by cytokines such as IL-5 and CXCL8, which mediate chemotaxis and degranulation. Unlike isolated neutrophilic inflammation characterized predominantly by IL-8 and TNF-a signaling, the combined response amplifies tissue damage through enhanced release of reactive oxygen species, proteases, and eosinophil-derived neurotoxins. This pathophysiology underpins chronic inflammatory diseases like asthma and certain infections, where mixed granulocyte infiltration exacerbates airway remodeling and hypersensitivity.
Clinical Significance: Neutrophilic vs Neutrophilic Eosinophilic Patterns
Neutrophilic patterns, characterized by elevated neutrophil counts, indicate acute bacterial infections or inflammatory conditions such as sepsis and pneumonia, guiding antibiotic therapy decisions. Neutrophilic eosinophilic patterns, showing concurrent increases in neutrophils and eosinophils, often suggest complex allergic reactions or parasitic infections, requiring targeted anti-inflammatory or antiparasitic treatment. Recognizing these distinct hematologic profiles enhances diagnostic accuracy and optimizes clinical management in respiratory and systemic diseases.
Diagnostic Criteria and Biomarkers
Neutrophilic eosinophilic inflammation is characterized by the coexistence of elevated neutrophils and eosinophils in tissue or sputum, whereas neutrophilic inflammation shows predominantly increased neutrophils without significant eosinophil elevation. Diagnostic criteria for neutrophilic eosinophilic conditions often include sputum analysis revealing neutrophil counts above 60% combined with eosinophil counts exceeding 3%, alongside clinical features suggestive of mixed-type airway inflammation. Key biomarkers differentiating these conditions involve elevated myeloperoxidase and neutrophil elastase for neutrophilic inflammation, while eosinophilic markers such as eosinophil cationic protein and periostin help identify the eosinophilic component within mixed inflammatory profiles.
Therapeutic Approaches for Different Inflammatory Types
Therapeutic approaches for neutrophilic eosinophilic inflammation often combine corticosteroids to reduce eosinophilic activity and macrolide antibiotics to target neutrophilic inflammation, effectively managing mixed cellular profiles. Neutrophilic inflammation typically requires treatments focused on antibiotics, immunomodulators like macrolides, and biologics such as anti-IL-17 agents to control neutrophil-driven inflammation and reduce tissue damage. Tailoring therapy based on the dominant inflammatory cell type enhances treatment efficacy and minimizes adverse effects by addressing specific cytokine pathways and immune responses characteristic of each inflammation phenotype.
Future Research Directions and Clinical Implications
Future research directions on neutrophilic eosinophilic versus neutrophilic inflammation emphasize identifying distinct molecular pathways and immune responses to develop targeted therapies. Clinical implications include improved diagnostic criteria and personalized treatment plans that address the differential roles of neutrophils and eosinophils in chronic inflammatory diseases such as asthma and COPD. Enhanced understanding of these cellular interactions could lead to novel biomarkers and more effective anti-inflammatory drugs tailored to patient-specific inflammatory profiles.
Neutrophilic Eosinophilic Infographic
 libterm.com
libterm.com