Sialadenitis is the inflammation of the salivary glands, often caused by infection or autoimmune disorders, while Sjogren's Syndrome is a chronic autoimmune condition that primarily targets these glands, leading to dry mouth and other systemic symptoms. Managing these conditions requires early diagnosis and appropriate treatment to prevent complications such as glandular damage or secondary infections. Explore the rest of the article to understand the symptoms, diagnosis, and effective management strategies for sialadenitis and Sjogren's Syndrome.
Table of Comparison
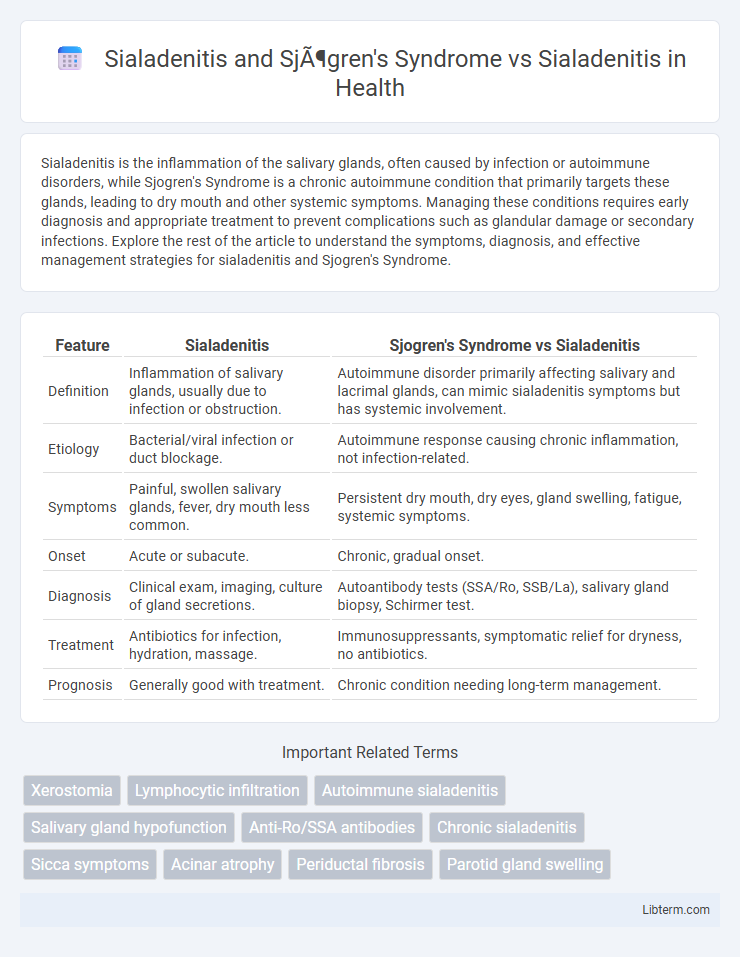
| Feature | Sialadenitis | Sjogren's Syndrome vs Sialadenitis |
|---|---|---|
| Definition | Inflammation of salivary glands, usually due to infection or obstruction. | Autoimmune disorder primarily affecting salivary and lacrimal glands, can mimic sialadenitis symptoms but has systemic involvement. |
| Etiology | Bacterial/viral infection or duct blockage. | Autoimmune response causing chronic inflammation, not infection-related. |
| Symptoms | Painful, swollen salivary glands, fever, dry mouth less common. | Persistent dry mouth, dry eyes, gland swelling, fatigue, systemic symptoms. |
| Onset | Acute or subacute. | Chronic, gradual onset. |
| Diagnosis | Clinical exam, imaging, culture of gland secretions. | Autoantibody tests (SSA/Ro, SSB/La), salivary gland biopsy, Schirmer test. |
| Treatment | Antibiotics for infection, hydration, massage. | Immunosuppressants, symptomatic relief for dryness, no antibiotics. |
| Prognosis | Generally good with treatment. | Chronic condition needing long-term management. |
Overview of Sialadenitis
Sialadenitis is an inflammatory condition of the salivary glands often caused by bacterial infection, leading to pain, swelling, and sometimes fever. Sjogren's Syndrome, an autoimmune disorder, frequently results in chronic sialadenitis by targeting salivary glands and causing persistent dry mouth and gland inflammation. Differentiating between infectious sialadenitis and autoimmune-related sialadenitis in Sjogren's Syndrome is critical for diagnosis and tailored treatment strategies.
Understanding Sjögren's Syndrome
Sialadenitis presents as inflammation of the salivary glands often caused by bacterial or viral infections, whereas Sjogren's Syndrome is an autoimmune disorder primarily targeting exocrine glands, leading to chronic inflammation and glandular dysfunction. Understanding Sjogren's Syndrome involves recognizing its hallmark symptoms of dry mouth (xerostomia) and dry eyes (keratoconjunctivitis sicca), which arise from lymphocytic infiltration and destruction of salivary and lacrimal glands. Diagnostic evaluation typically includes serological markers such as anti-SSA/Ro and anti-SSB/La antibodies, salivary gland biopsy, and tests for glandular function, distinguishing it from infectious or obstructive causes of sialadenitis.
Pathophysiology: Sialadenitis vs. Sjögren’s Syndrome
Sialadenitis involves acute or chronic inflammation of the salivary glands primarily due to bacterial or viral infections causing ductal obstruction and glandular swelling, often with neutrophilic infiltration. Sjogren's Syndrome is an autoimmune disorder characterized by lymphocytic infiltration and destruction of exocrine glands, particularly the salivary and lacrimal glands, resulting in xerostomia and keratoconjunctivitis sicca. The pathophysiology of Sjogren's involves chronic immune-mediated epithelial cell damage, autoantibody production, and systemic manifestations, differing fundamentally from the infection-driven inflammation seen in typical sialadenitis.
Common Causes of Sialadenitis
Sialadenitis, characterized by inflammation of the salivary glands, commonly arises from bacterial infections such as Staphylococcus aureus and viral infections like mumps virus, alongside ductal obstruction from salivary stones. Sjogren's Syndrome-related sialadenitis distinguishes itself as an autoimmune disorder causing chronic lymphocytic infiltration and glandular dysfunction, differing from the primarily infectious or obstructive etiologies seen in typical sialadenitis. Understanding these causes is crucial for accurate diagnosis, highlighting that while common sialadenitis often results from infection or blockage, Sjogren's Syndrome involves systemic autoimmune pathology.
Clinical Manifestations and Symptoms Comparison
Sialadenitis presents primarily with unilateral or bilateral salivary gland swelling, pain, erythema, and sometimes purulent discharge, predominantly affecting the parotid or submandibular glands due to bacterial infection or obstruction. Sjogren's Syndrome-related sialadenitis typically manifests as chronic, symmetric salivary gland enlargement accompanied by xerostomia (dry mouth), mucosal dryness, and systemic autoimmune features such as fatigue, arthralgia, and lymphocytic infiltration on biopsy. Unlike acute bacterial sialadenitis, Sjogren's Syndrome involves systemic autoimmune symptoms and persistent gland dysfunction, leading to more widespread dryness and systemic immune-related complications.
Diagnostic Approaches for Sialadenitis and Sjögren’s Syndrome
Diagnostic approaches for Sialadenitis and Sjogren's Syndrome involve salivary gland imaging, serological tests, and histopathological examination. Ultrasound and MRI help detect glandular swelling and inflammation in both conditions, while blood tests for autoantibodies such as anti-SSA/Ro and anti-SSB/La are critical for identifying Sjogren's Syndrome. Minor salivary gland biopsy showing focal lymphocytic sialadenitis confirms Sjogren's Syndrome, whereas bacterial cultures and clinical presentation primarily guide Sialadenitis diagnosis.
Imaging and Laboratory Findings: A Comparative Review
Sialadenitis associated with Sjogren's Syndrome typically presents with bilateral parotid gland enlargement on imaging modalities such as ultrasound and MRI, showing heterogeneous echotexture and multiple hypoechoic areas reflecting lymphocytic infiltration and glandular atrophy. Laboratory findings in Sjogren's-related sialadenitis often include positive anti-Ro/SSA and anti-La/SSB autoantibodies, elevated erythrocyte sedimentation rate (ESR), and hypergammaglobulinemia, distinguishing it from non-autoimmune sialadenitis, which generally shows localized inflammation with elevated white blood cell count and normal autoimmune markers. Contrast-enhanced imaging and serological tests are critical in differentiating Sjogren's Syndrome from infectious or obstructive sialadenitis, guiding appropriate immunomodulatory versus antimicrobial therapy.
Treatment Strategies: Sialadenitis vs. Sjögren’s Syndrome-Related Sialadenitis
Treatment strategies for sialadenitis primarily involve antibiotic therapy targeting bacterial infections, hydration, and massage to promote salivary flow. In contrast, Sjogren's syndrome-related sialadenitis requires immunomodulatory treatments such as corticosteroids or disease-modifying antirheumatic drugs (DMARDs) to address autoimmune inflammation alongside symptom management like artificial saliva and pain relief. While sialadenitis treatment focuses on infection control, Sjogren's syndrome-related approaches center on controlling systemic autoimmune responses and preserving gland function.
Prognosis and Complications
Sialadenitis associated with Sjogren's Syndrome often presents a chronic course with increased risk of glandular atrophy and lymphoma development, leading to a generally poorer prognosis compared to isolated sialadenitis, which is typically acute and resolves with appropriate antimicrobial therapy. Complications of Sjogren's-related sialadenitis include persistent xerostomia, recurrent infections, and systemic manifestations such as interstitial lung disease and arthritis, whereas uncomplicated sialadenitis rarely progresses beyond localized inflammation and abscess formation. Management strategies must consider the autoimmune etiology in Sjogren's Syndrome to prevent long-term glandular damage and systemic involvement, contrasting with the usually straightforward treatment of bacterial sialadenitis.
Key Differences and Similarities: Sialadenitis vs. Sjögren’s Syndrome
Sialadenitis refers to acute or chronic inflammation of the salivary glands often caused by bacterial or viral infections, whereas Sjogren's Syndrome is a chronic autoimmune disorder characterized by lymphocytic infiltration and destruction of exocrine glands, primarily salivary and lacrimal glands. Both conditions share symptoms like dry mouth (xerostomia) and gland swelling but differ in etiology, with Sialadenitis linked to infectious agents and Sjogren's involving systemic autoimmune mechanisms. Treatment for Sialadenitis focuses on infection control with antibiotics and hydration, while Sjogren's Syndrome requires immunomodulatory therapies to manage chronic gland dysfunction and systemic manifestations.
Sialadenitis and Sjögren's Syndrome Infographic
 libterm.com
libterm.com