Adrenal insufficiency is a condition where the adrenal glands produce insufficient amounts of essential hormones like cortisol and aldosterone, leading to symptoms such as fatigue, muscle weakness, and low blood pressure. Proper diagnosis and treatment are critical to managing this disorder and avoiding life-threatening complications. Explore the rest of the article to understand how adrenal insufficiency affects your health and the options available for effective management.
Table of Comparison
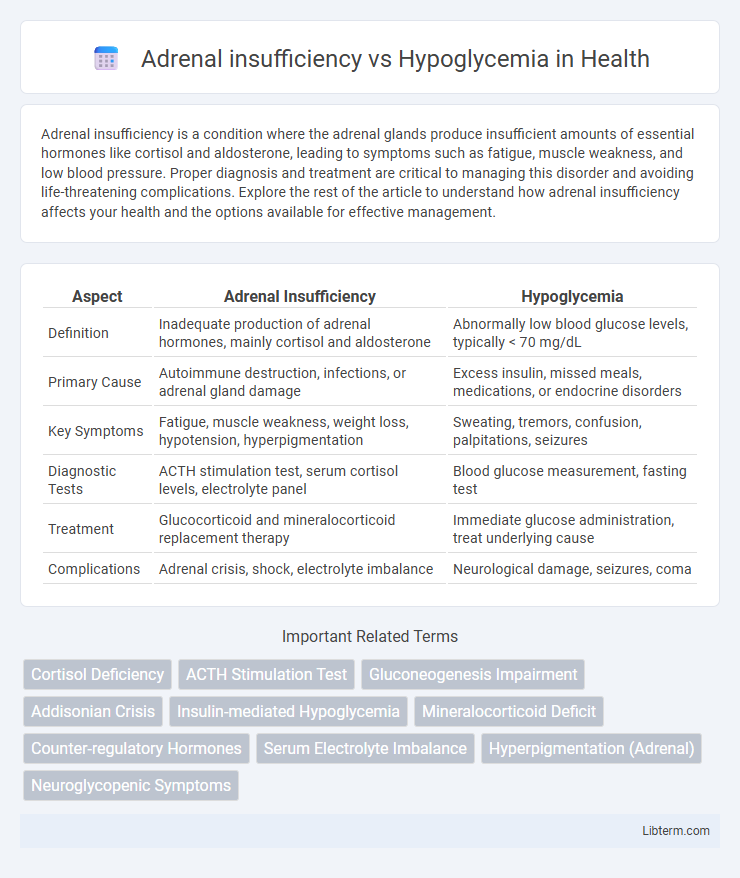
| Aspect | Adrenal Insufficiency | Hypoglycemia |
|---|---|---|
| Definition | Inadequate production of adrenal hormones, mainly cortisol and aldosterone | Abnormally low blood glucose levels, typically < 70 mg/dL |
| Primary Cause | Autoimmune destruction, infections, or adrenal gland damage | Excess insulin, missed meals, medications, or endocrine disorders |
| Key Symptoms | Fatigue, muscle weakness, weight loss, hypotension, hyperpigmentation | Sweating, tremors, confusion, palpitations, seizures |
| Diagnostic Tests | ACTH stimulation test, serum cortisol levels, electrolyte panel | Blood glucose measurement, fasting test |
| Treatment | Glucocorticoid and mineralocorticoid replacement therapy | Immediate glucose administration, treat underlying cause |
| Complications | Adrenal crisis, shock, electrolyte imbalance | Neurological damage, seizures, coma |
Overview of Adrenal Insufficiency and Hypoglycemia
Adrenal insufficiency is characterized by the inadequate production of cortisol and aldosterone due to adrenal gland dysfunction, leading to symptoms like fatigue, muscle weakness, and hypotension. Hypoglycemia occurs when blood glucose levels drop below normal ranges, causing symptoms such as shakiness, sweating, confusion, and, in severe cases, loss of consciousness. Both conditions require timely diagnosis but differ fundamentally in hormonal imbalance and clinical management strategies.
Causes of Adrenal Insufficiency
Adrenal insufficiency primarily results from autoimmune destruction of the adrenal cortex, infections like tuberculosis, or adrenal hemorrhage causing impaired cortisol and aldosterone production. Secondary adrenal insufficiency arises due to pituitary gland dysfunction, leading to inadequate adrenocorticotropic hormone (ACTH) stimulation. This contrasts with hypoglycemia, which stems from excessive insulin, prolonged fasting, or endocrine disorders but does not typically involve adrenal hormone deficits.
Causes of Hypoglycemia
Hypoglycemia primarily results from excessive insulin administration, inadequate food intake, prolonged fasting, or intense physical activity, which disrupt glucose homeostasis. Other causes include endocrine disorders like adrenal insufficiency and hypopituitarism that reduce counter-regulatory hormone levels, impairing glucose production. Medications such as sulfonylureas and conditions like insulinoma also contribute to hypoglycemia by increasing insulin levels or enhancing insulin sensitivity.
Key Symptoms: Comparing Presentations
Adrenal insufficiency typically presents with fatigue, muscle weakness, weight loss, hypotension, and hyperpigmentation, while hypoglycemia is characterized by shakiness, sweating, palpitations, and confusion. Both conditions may share symptoms like confusion and weakness, but hypoglycemia often includes rapid onset neuroglycopenic symptoms such as irritability and seizures. Distinguishing features include persistent low blood glucose in hypoglycemia versus electrolyte imbalances and cortisol deficiency in adrenal insufficiency.
Pathophysiological Differences
Adrenal insufficiency results from inadequate cortisol production, impairing gluconeogenesis and reducing the body's ability to maintain fasting blood glucose levels. Hypoglycemia primarily involves excessive insulin action or glucose utilization, leading to abnormally low blood glucose independent of adrenal gland function. While adrenal insufficiency disrupts hormonal regulation of glucose homeostasis, hypoglycemia reflects an imbalance between glucose supply and cellular uptake.
Diagnostic Approaches for Each Condition
Diagnostic approaches for adrenal insufficiency involve measuring serum cortisol and adrenocorticotropic hormone (ACTH) levels, with the ACTH stimulation test serving as the gold standard to assess adrenal gland function. In contrast, hypoglycemia diagnosis relies on documenting low plasma glucose levels during symptomatic episodes, with supportive tests including insulin, C-peptide, and beta-hydroxybutyrate measurements to identify the underlying cause. Both conditions require careful evaluation of biochemical markers and clinical presentation to differentiate and confirm diagnosis accurately.
Risk Factors and Predisposing Conditions
Adrenal insufficiency risk factors include autoimmune disorders such as Addison's disease, infections like tuberculosis, and chronic corticosteroid use leading to hypothalamic-pituitary-adrenal axis suppression. Hypoglycemia predisposes individuals with diabetes mellitus, particularly those on insulin or sulfonylureas, and those with critical conditions such as liver failure or sepsis. Both conditions share overlapping symptoms but require distinct management based on their underlying etiologies and risk profiles.
Acute Management Strategies
Acute management of adrenal insufficiency requires immediate administration of intravenous hydrocortisone and aggressive fluid resuscitation to correct hypotension and electrolyte imbalances. In contrast, hypoglycemia demands prompt glucose replacement, either orally if the patient is conscious or intravenously via dextrose infusion in severe cases to rapidly restore normal blood sugar levels. Both conditions necessitate continuous monitoring of vital signs and laboratory parameters to prevent complications and ensure stabilizing metabolic function.
Long-Term Treatment Considerations
Long-term treatment for adrenal insufficiency often requires lifelong glucocorticoid and mineralocorticoid replacement therapy to maintain hormone balance and prevent adrenal crises. In contrast, managing hypoglycemia involves continuous glucose monitoring and tailored dietary adjustments to regulate blood sugar levels and prevent severe episodes. Both conditions necessitate ongoing patient education and regular medical follow-up to optimize treatment efficacy and minimize complications.
Prevention and Patient Education
Preventing adrenal insufficiency involves regular monitoring of cortisol levels and adherence to prescribed glucocorticoid therapy, particularly during stress or illness to avoid adrenal crisis. Patients should receive education on recognizing early symptoms such as fatigue, dizziness, and nausea, and the importance of carrying emergency hydrocortisone injection kits. In hypoglycemia prevention, diabetic patients need comprehensive training on blood glucose monitoring, balanced meal planning, medication timing, and recognizing signs like sweating, shakiness, and confusion to promptly manage low blood sugar episodes.
Adrenal insufficiency Infographic
 libterm.com
libterm.com