Insulinoma is a rare pancreatic tumor that causes excessive insulin production, leading to hypoglycemia and symptoms such as confusion, sweating, and weakness. Accurate diagnosis typically involves blood tests and imaging studies to detect the tumor and monitor glucose levels. Discover how understanding insulinoma's signs and treatment options can help you manage this condition effectively by reading the full article.
Table of Comparison
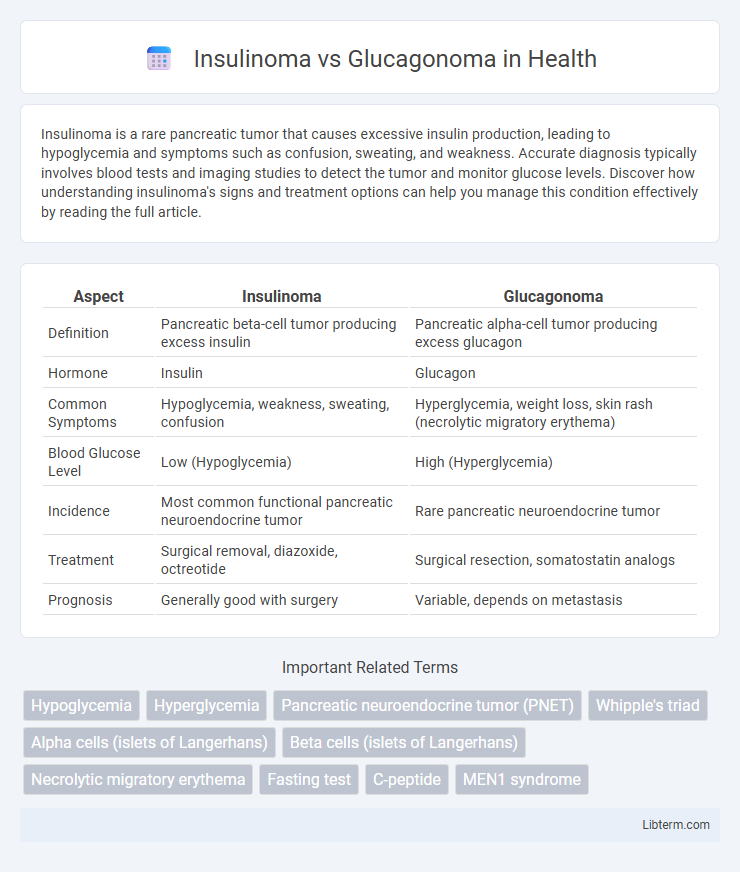
| Aspect | Insulinoma | Glucagonoma |
|---|---|---|
| Definition | Pancreatic beta-cell tumor producing excess insulin | Pancreatic alpha-cell tumor producing excess glucagon |
| Hormone | Insulin | Glucagon |
| Common Symptoms | Hypoglycemia, weakness, sweating, confusion | Hyperglycemia, weight loss, skin rash (necrolytic migratory erythema) |
| Blood Glucose Level | Low (Hypoglycemia) | High (Hyperglycemia) |
| Incidence | Most common functional pancreatic neuroendocrine tumor | Rare pancreatic neuroendocrine tumor |
| Treatment | Surgical removal, diazoxide, octreotide | Surgical resection, somatostatin analogs |
| Prognosis | Generally good with surgery | Variable, depends on metastasis |
Introduction to Insulinoma and Glucagonoma
Insulinoma and glucagonoma are rare pancreatic neuroendocrine tumors originating from islet cells, with insulinoma arising from beta cells and glucagonoma from alpha cells. Insulinomas predominantly cause hypoglycemia due to excessive insulin secretion, while glucagonomas lead to hyperglycemia and characteristic skin rash caused by increased glucagon levels. Both tumors require biochemical testing and imaging for accurate diagnosis and differ significantly in clinical presentation and metabolic effects.
Pathophysiology: Insulinoma vs Glucagonoma
Insulinomas are pancreatic neuroendocrine tumors that secrete excessive insulin, causing hypoglycemia by promoting glucose uptake in peripheral tissues and inhibiting hepatic glucose production. In contrast, glucagonomas produce excess glucagon, leading to hyperglycemia through increased gluconeogenesis and glycogenolysis in the liver, along with lipolysis. The pathophysiological imbalance in insulinomas results in neuroglycopenic symptoms, whereas glucagonomas cause dermatologic manifestations like necrolytic migratory erythema and weight loss due to catabolic effects.
Epidemiology and Risk Factors
Insulinomas are rare pancreatic neuroendocrine tumors with an incidence of 1-4 cases per million annually, commonly affecting adults aged 40-60, with a slight female predominance. Glucagonomas are even rarer, occurring in approximately 1 case per 20 million people per year, typically presenting in middle-aged adults, and are often associated with a genetic predisposition such as multiple endocrine neoplasia type 1 (MEN1). Both tumors share risk factors related to MEN1 syndrome, but insulinomas primarily arise sporadically, while glucagonomas demonstrate a stronger link to hereditary conditions.
Clinical Presentation: Signs and Symptoms
Insulinoma typically presents with episodes of hypoglycemia characterized by sweating, confusion, palpitations, and seizures due to excessive insulin secretion. Glucagonoma manifests through hyperglycemia, necrolytic migratory erythema, weight loss, and anemia caused by elevated glucagon levels. Distinguishing clinical signs such as Whipple's triad in insulinoma and characteristic skin rash in glucagonoma aid in differential diagnosis.
Diagnostic Criteria and Laboratory Findings
Insulinoma diagnosis is primarily based on supervised fasting tests showing inappropriately high insulin levels (>3 mU/mL), low plasma glucose (<50 mg/dL), and increased C-peptide levels, confirming endogenous hyperinsulinemia. Glucagonoma is characterized by elevated serum glucagon concentrations (>500 pg/mL) along with hyperglycemia, weight loss, and necrolytic migratory erythema, with diagnostic imaging identifying pancreatic alpha-cell tumors. Both tumors require biochemical assays combined with imaging studies such as CT or MRI for precise localization and confirmation.
Imaging and Localization Techniques
Insulinomas typically localize within the pancreas and are best visualized using multiphase contrast-enhanced CT or MRI, which highlight their hypervascular nature during the arterial phase. Endoscopic ultrasound provides high sensitivity for detecting small insulinomas and facilitates fine-needle aspiration for histopathological confirmation. Glucagonomas, often larger and more necrotic, are similarly identified by contrast-enhanced imaging, but somatostatin receptor scintigraphy and 68Ga-DOTATATE PET/CT offer superior sensitivity for detecting metastatic sites and assessing somatostatin receptor expression.
Differential Diagnosis
Insulinoma and glucagonoma are rare pancreatic neuroendocrine tumors with distinct biochemical profiles; insulinomas primarily secrete insulin causing hypoglycemia, whereas glucagonomas secrete glucagon leading to hyperglycemia and characteristic necrolytic migratory erythema. Differential diagnosis relies on measuring plasma insulin, C-peptide, and glucose levels for insulinoma, contrasted with elevated glucagon levels and clinical features such as weight loss and diabetes in glucagonoma. Imaging studies, including endoscopic ultrasound and somatostatin receptor scintigraphy, assist in localizing tumors and distinguishing between these functional syndromes.
Treatment Approaches: Medical and Surgical Options
Treatment of insulinoma primarily involves surgical resection, which is often curative, while medical management with diazoxide or octreotide is reserved for inoperable cases or symptom control. Glucagonoma treatment centers on tumor resection as well, supplemented by somatostatin analogs such as octreotide to manage glucagon hypersecretion symptoms and streptozocin-based chemotherapy for metastatic disease. Both conditions may require combination therapies including nutritional support and glucose monitoring to address hormone-related metabolic imbalances.
Prognosis and Complications
Insulinomas typically have a favorable prognosis due to their benign nature and effective surgical resection, while glucagonomas often present a worse prognosis because of delayed diagnosis and malignant potential. Complications of insulinomas include recurrent hypoglycemia leading to neurological damage, whereas glucagonomas cause severe hyperglycemia, weight loss, and necrolytic migratory erythema. Both tumors require early detection to minimize metabolic derangements and improve patient outcomes.
Summary: Key Differences and Clinical Implications
Insulinomas are rare pancreatic neuroendocrine tumors that cause hypoglycemia due to excessive insulin secretion, whereas glucagonomas lead to hyperglycemia through overproduction of glucagon. Clinically, insulinoma patients present with neuroglycopenic symptoms such as confusion and sweating, while glucagonoma features include necrolytic migratory erythema, weight loss, and diabetes mellitus. Accurate differentiation between these tumors is critical for targeted surgical intervention and management of metabolic complications.
Insulinoma Infographic
 libterm.com
libterm.com