Pneumonia is a lung infection caused by bacteria, viruses, or fungi, leading to inflammation and fluid buildup in the air sacs, which impairs breathing. Symptoms often include cough, fever, chest pain, and difficulty breathing, requiring prompt medical evaluation to prevent complications. Discover essential information about pneumonia's causes, symptoms, treatment, and prevention to protect your health by reading the full article.
Table of Comparison
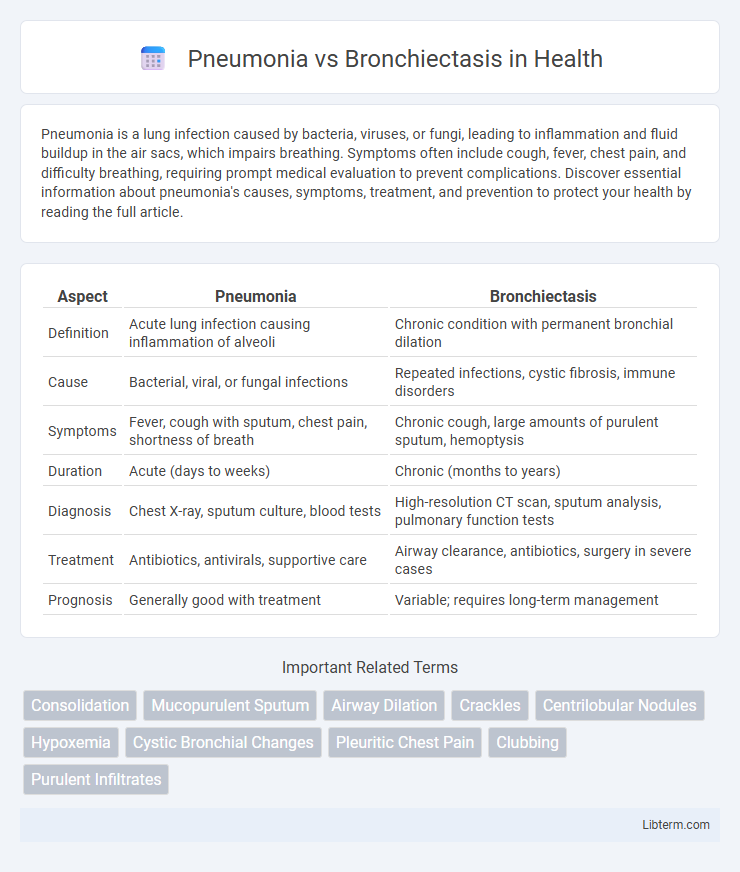
| Aspect | Pneumonia | Bronchiectasis |
|---|---|---|
| Definition | Acute lung infection causing inflammation of alveoli | Chronic condition with permanent bronchial dilation |
| Cause | Bacterial, viral, or fungal infections | Repeated infections, cystic fibrosis, immune disorders |
| Symptoms | Fever, cough with sputum, chest pain, shortness of breath | Chronic cough, large amounts of purulent sputum, hemoptysis |
| Duration | Acute (days to weeks) | Chronic (months to years) |
| Diagnosis | Chest X-ray, sputum culture, blood tests | High-resolution CT scan, sputum analysis, pulmonary function tests |
| Treatment | Antibiotics, antivirals, supportive care | Airway clearance, antibiotics, surgery in severe cases |
| Prognosis | Generally good with treatment | Variable; requires long-term management |
Introduction to Pneumonia and Bronchiectasis
Pneumonia is an acute respiratory infection characterized by inflammation of the alveoli and air sacs in the lungs, commonly caused by bacterial, viral, or fungal pathogens. Bronchiectasis is a chronic lung condition marked by permanent dilation and damage of the bronchial tubes, leading to recurrent infections and impaired mucus clearance. Both conditions impair respiratory function but differ in pathophysiology, clinical presentation, and long-term management strategies.
Causes and Risk Factors
Pneumonia is primarily caused by bacterial, viral, or fungal infections that lead to lung inflammation, with risk factors including age extremes, weakened immune systems, and chronic illnesses such as COPD and heart disease. Bronchiectasis results from chronic or repeated lung infections and inflammation that damage the airway walls, with common causes being cystic fibrosis, tuberculosis, and immune system disorders, while risk factors involve a history of severe lung infections and genetic predisposition. Both conditions share overlapping risk factors like respiratory infections and immune deficiencies but differ fundamentally in their pathophysiology and etiology.
Pathophysiology: Key Differences
Pneumonia is characterized by acute inflammation of the alveoli due to infectious agents leading to alveolar consolidation and impaired gas exchange, whereas bronchiectasis involves chronic inflammation and irreversible dilation of the bronchi resulting from repeated infection or obstruction. In pneumonia, the pathophysiology centers on the filling of alveolar spaces with exudate, while bronchiectasis features destruction of bronchial walls and impaired mucociliary clearance causing mucus retention and recurrent infections. These distinct mechanisms underlie the different clinical presentations and treatment approaches for both respiratory conditions.
Clinical Manifestations and Symptoms
Pneumonia typically presents with acute symptoms such as high fever, productive cough with purulent sputum, chest pain, and dyspnea, often accompanied by systemic signs like chills and fatigue. Bronchiectasis features chronic symptoms including persistent productive cough with large amounts of foul-smelling sputum, recurrent respiratory infections, and hemoptysis, along with breathlessness and wheezing. Both conditions involve cough and respiratory distress, but pneumonia manifests acutely, whereas bronchiectasis presents with long-standing, recurrent respiratory symptoms.
Diagnostic Criteria and Procedures
Pneumonia diagnosis primarily relies on clinical presentation, chest X-rays showing localized lung infiltrates, and sputum culture identifying causative pathogens. Bronchiectasis diagnosis involves high-resolution computed tomography (HRCT) scans revealing bronchial dilation and wall thickening, alongside sputum analysis for chronic infection and pulmonary function tests assessing airflow limitation. Both conditions require microbiological testing but differ significantly in imaging features and chronicity assessment.
Imaging and Laboratory Findings
Pneumonia typically presents on imaging with localized alveolar consolidation, air bronchograms, and potential pleural effusions, while bronchiectasis is characterized by bronchial wall thickening, dilated airways, and tram-track or signet-ring appearances on high-resolution CT scans. Laboratory findings in pneumonia often reveal elevated inflammatory markers such as C-reactive protein (CRP) and leukocytosis with neutrophilia, whereas bronchiectasis may show chronic inflammation markers, elevated sputum cultures with persistent bacterial colonization, and mild leukocytosis. Distinguishing features include the acute onset and systemic inflammatory response in pneumonia versus the chronic, recurrent infection pattern and structural airway damage seen in bronchiectasis.
Treatment Approaches and Therapies
Pneumonia treatment primarily involves targeted antibiotic therapy based on the causative pathogen, along with supportive care such as oxygen therapy and hydration to improve lung function and reduce inflammation. Bronchiectasis management focuses on long-term airway clearance techniques, including chest physiotherapy and inhaled bronchodilators, combined with chronic antibiotic regimens to prevent recurrent infections and control mucus buildup. Both conditions may require corticosteroids or immunomodulatory agents in severe cases to reduce airway inflammation and improve respiratory outcomes.
Complications and Prognosis
Pneumonia complications often include pleural effusion, lung abscess, respiratory failure, and sepsis, with prognosis generally favorable if treated promptly but worsening significantly in elderly or immunocompromised patients. Bronchiectasis complications involve recurrent lung infections, hemoptysis, and progressive respiratory decline due to irreversible airway dilation, resulting in a chronic condition with variable prognosis dependent on underlying cause and treatment adherence. Long-term management in bronchiectasis can improve quality of life and reduce exacerbations, whereas pneumonia prognosis hinges on timely antibiotic therapy and addressing risk factors.
Prevention Strategies
Effective prevention of pneumonia involves vaccination against Streptococcus pneumoniae and influenza, maintaining proper hand hygiene, and avoiding smoking to reduce respiratory tract vulnerability. Bronchiectasis prevention emphasizes early treatment of lung infections, regular airway clearance techniques, and management of underlying conditions like cystic fibrosis or immune deficiencies. Both conditions benefit from healthy lifestyle practices, including adequate nutrition and prompt medical attention for respiratory symptoms.
Summary: Pneumonia vs Bronchiectasis
Pneumonia is an acute infection causing inflammation of the lung parenchyma, characterized by symptoms like fever, cough, and chest pain, often confirmed through chest X-rays showing consolidation. Bronchiectasis is a chronic condition marked by permanent dilation and damage of the bronchi, leading to persistent cough, sputum production, and recurrent respiratory infections, with high-resolution CT scans revealing bronchial wall thickening and dilatation. Both conditions impact respiratory health but differ in pathophysiology, clinical presentation, imaging, and long-term management strategies.
Pneumonia Infographic
 libterm.com
libterm.com