Narcolepsy is a chronic neurological disorder characterized by overwhelming daytime sleepiness and sudden sleep attacks that can disrupt daily life. Symptoms include excessive daytime fatigue, cataplexy (sudden muscle weakness), sleep paralysis, and hallucinations, all due to abnormal regulation of REM sleep. Learn more about narcolepsy's causes, symptoms, and treatments to better manage Your condition and improve quality of life.
Table of Comparison
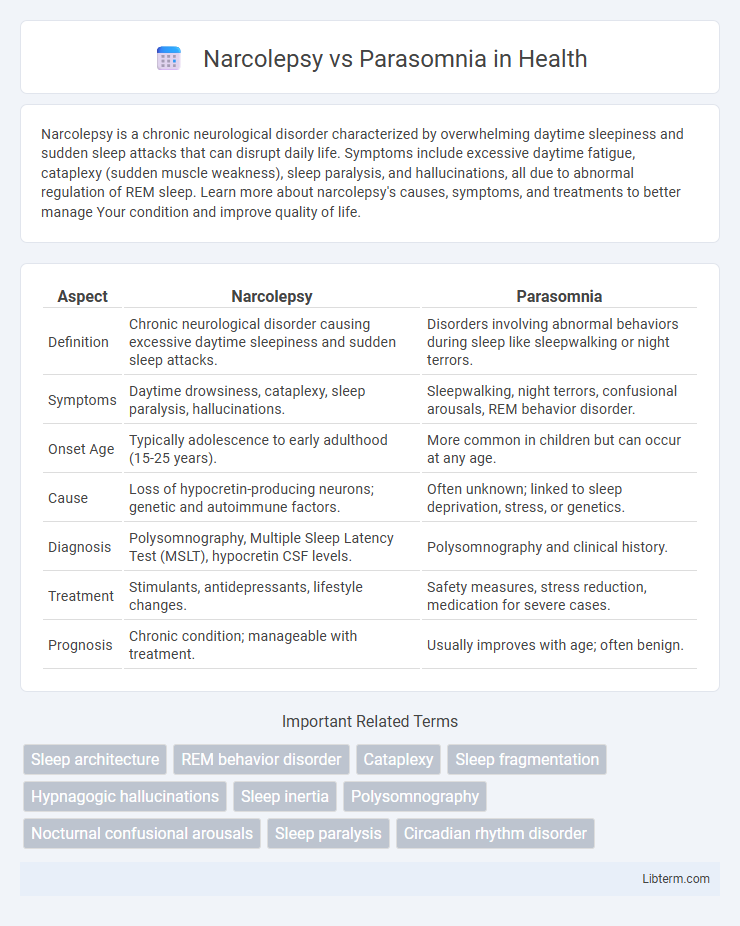
| Aspect | Narcolepsy | Parasomnia |
|---|---|---|
| Definition | Chronic neurological disorder causing excessive daytime sleepiness and sudden sleep attacks. | Disorders involving abnormal behaviors during sleep like sleepwalking or night terrors. |
| Symptoms | Daytime drowsiness, cataplexy, sleep paralysis, hallucinations. | Sleepwalking, night terrors, confusional arousals, REM behavior disorder. |
| Onset Age | Typically adolescence to early adulthood (15-25 years). | More common in children but can occur at any age. |
| Cause | Loss of hypocretin-producing neurons; genetic and autoimmune factors. | Often unknown; linked to sleep deprivation, stress, or genetics. |
| Diagnosis | Polysomnography, Multiple Sleep Latency Test (MSLT), hypocretin CSF levels. | Polysomnography and clinical history. |
| Treatment | Stimulants, antidepressants, lifestyle changes. | Safety measures, stress reduction, medication for severe cases. |
| Prognosis | Chronic condition; manageable with treatment. | Usually improves with age; often benign. |
Understanding Narcolepsy and Parasomnia
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations, affecting the brain's ability to regulate sleep-wake cycles. Parasomnia refers to a group of sleep disorders involving abnormal movements, behaviors, emotions, perceptions, or dreams during transitions between sleep stages, including sleepwalking, night terrors, and REM sleep behavior disorder. Differentiating narcolepsy from parasomnias involves evaluating symptoms' timing, frequency, and associated neurological features to ensure accurate diagnosis and effective treatment.
Key Differences Between Narcolepsy and Parasomnia
Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness, sudden muscle weakness (cataplexy), and disrupted nighttime sleep, while parasomnia involves abnormal behaviors or experiences during sleep, such as sleepwalking, night terrors, or REM sleep behavior disorder. Narcolepsy primarily affects the brain's ability to regulate the sleep-wake cycle, often linked to hypocretin deficiency, whereas parasomnias arise from partial arousals during non-REM or REM sleep stages without impacting sleep-wake regulation. Diagnosis of narcolepsy relies on polysomnography and multiple sleep latency tests, whereas parasomnias are typically identified through clinical history and sleep studies focusing on abnormal movements or vocalizations during sleep.
Causes of Narcolepsy vs Parasomnia
Narcolepsy primarily results from a deficiency of the neurotransmitter hypocretin (orexin), often linked to autoimmune destruction of hypothalamic neurons. Parasomnias arise from disruptions during sleep transitions, involving abnormal activation patterns in the brain, with causes including genetic predisposition, stress, and certain medications. Understanding these distinct pathophysiological mechanisms is essential for accurate diagnosis and targeted treatment of narcolepsy versus parasomnia.
Common Symptoms of Narcolepsy
Narcolepsy commonly presents with excessive daytime sleepiness, cataplexy, sleep paralysis, and hypnagogic hallucinations, which distinguish it from parasomnias that involve abnormal behaviors during sleep such as sleepwalking or night terrors. Patients with narcolepsy experience sudden muscle weakness triggered by strong emotions, unlike parasomnia episodes that occur primarily during non-REM sleep. Diagnosing narcolepsy requires polysomnography and multiple sleep latency tests to confirm abnormal REM sleep patterns and sleep onset latency.
Common Symptoms of Parasomnia
Parasomnia encompasses a range of sleep disorders characterized by abnormal behaviors, movements, emotions, perceptions, and dreams during sleep transitions. Common symptoms include sleepwalking, night terrors, confusional arousals, and acting out vivid dreams. Unlike narcolepsy, which primarily presents with excessive daytime sleepiness and sudden muscle weakness (cataplexy), parasomnia symptoms occur during specific sleep stages and often involve complex motor activities.
Diagnosis and Evaluation Methods
Narcolepsy diagnosis relies heavily on polysomnography followed by the Multiple Sleep Latency Test (MSLT) to measure daytime sleepiness and sleep onset rapid eye movement (REM) periods. Parasomnia evaluation also includes polysomnography but focuses on identifying abnormal behaviors during non-REM or REM sleep stages without the characteristic sleep onset REM episodes of narcolepsy. Clinical history, sleep diaries, and actigraphy further aid in differentiating narcolepsy from parasomnias by capturing symptom patterns and sleep architecture disturbances.
Treatment Approaches for Narcolepsy and Parasomnia
Treatment approaches for narcolepsy primarily involve stimulant medications such as modafinil and sodium oxybate to improve wakefulness and manage cataplexy symptoms. Parasomnia treatments vary depending on the specific disorder but often include behavioral interventions, ensuring safe sleep environments, and sometimes medications like benzodiazepines or antidepressants to reduce abnormal sleep behaviors. Both conditions benefit from a tailored treatment plan that addresses individual symptoms and improves overall sleep quality.
Impact on Daily Life and Quality of Sleep
Narcolepsy causes excessive daytime sleepiness and sudden sleep attacks, significantly disrupting daily activities and reducing overall productivity. Parasomnias involve abnormal behaviors during sleep, such as sleepwalking or night terrors, leading to fragmented sleep and increased risk of injury. Both conditions impair sleep quality, resulting in fatigue, cognitive difficulties, and diminished quality of life.
Risk Factors and Prevention Strategies
Narcolepsy is often linked to genetic predisposition and autoimmune factors, with risk increasing in individuals with a family history of the disorder, while parasomnia is commonly triggered by sleep deprivation, stress, and certain medications. Preventive strategies for narcolepsy include maintaining a consistent sleep schedule and managing autoimmune health, whereas parasomnia prevention involves improving sleep hygiene, reducing stress, and avoiding sleep-disrupting substances like alcohol and sedatives. Both conditions benefit from early diagnosis and personalized treatment plans to minimize symptoms and enhance overall sleep quality.
When to Seek Professional Help
Seek professional help for narcolepsy if experiencing excessive daytime sleepiness, sudden muscle weakness (cataplexy), or disrupted nighttime sleep that affects daily functioning. Parasomnia requires medical evaluation when behaviors like sleepwalking, violent movements, or frequent nightmares pose safety risks or cause significant distress. Early diagnosis and treatment improve management and reduce complications associated with these sleep disorders.
Narcolepsy Infographic
 libterm.com
libterm.com