Lichen planus is a chronic inflammatory condition that affects the skin, mouth, and other mucous membranes, presenting with itchy, flat-topped, purple lesions. This disorder often causes discomfort and potential complications, requiring accurate diagnosis and effective management to improve your quality of life. Explore the full article to learn about symptoms, causes, treatments, and preventive measures for lichen planus.
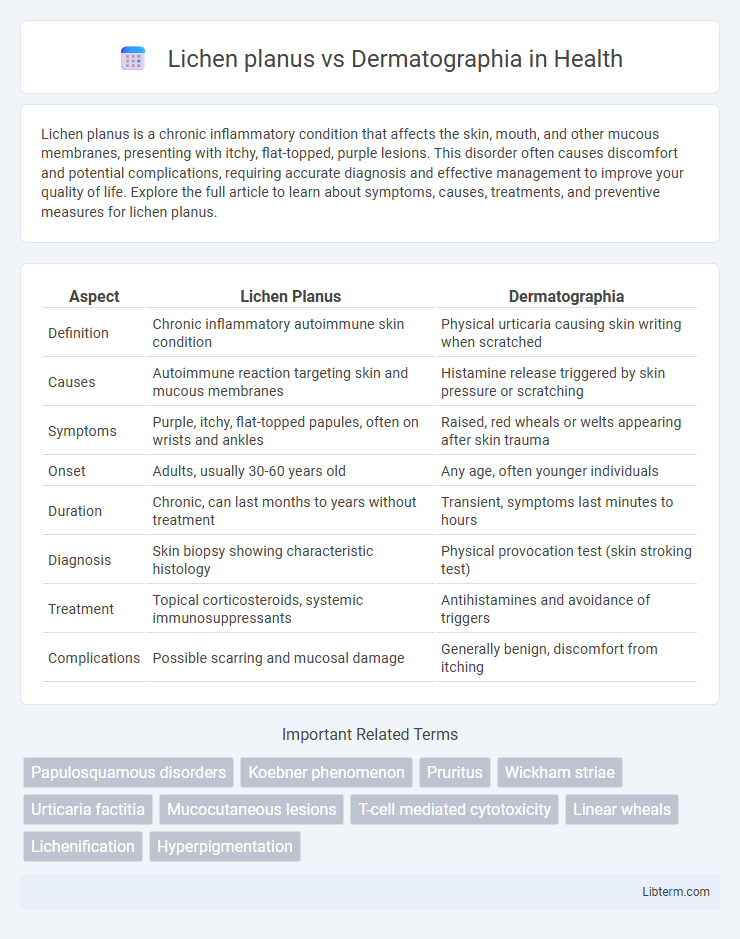
Table of Comparison
| Aspect | Lichen Planus | Dermatographia |
|---|---|---|
| Definition | Chronic inflammatory autoimmune skin condition | Physical urticaria causing skin writing when scratched |
| Causes | Autoimmune reaction targeting skin and mucous membranes | Histamine release triggered by skin pressure or scratching |
| Symptoms | Purple, itchy, flat-topped papules, often on wrists and ankles | Raised, red wheals or welts appearing after skin trauma |
| Onset | Adults, usually 30-60 years old | Any age, often younger individuals |
| Duration | Chronic, can last months to years without treatment | Transient, symptoms last minutes to hours |
| Diagnosis | Skin biopsy showing characteristic histology | Physical provocation test (skin stroking test) |
| Treatment | Topical corticosteroids, systemic immunosuppressants | Antihistamines and avoidance of triggers |
| Complications | Possible scarring and mucosal damage | Generally benign, discomfort from itching |
Understanding Lichen Planus: Definition and Causes
Lichen planus is a chronic inflammatory skin condition characterized by purplish, itchy, flat-topped papules often affecting the wrists, ankles, and mucous membranes, caused by an autoimmune response targeting skin and mucosal cells. The exact etiology involves T-cell mediated immune attack, frequently triggered by genetic predisposition, infections such as hepatitis C virus, certain medications, or exposure to allergens. Unlike dermatographia, which is a physical urticaria manifesting as transient wheals from skin scratching, lichen planus presents with persistent lesions and mucosal involvement, requiring immunomodulatory treatment.
What Is Dermatographia? An Overview
Dermatographia, also known as "skin writing," is a common skin condition characterized by raised, red lines or welts that appear after lightly scratching or stroking the skin, caused by an exaggerated histamine release. Unlike lichen planus, which is an inflammatory autoimmune disorder presenting with flat-topped, purple, itchy papules, dermatographia does not involve permanent lesions and typically resolves within 30 minutes. Diagnosis of dermatographia is clinical, based on the appearance of wheals following mechanical pressure, and treatment often includes antihistamines to control symptoms.
Key Differences Between Lichen Planus and Dermatographia
Lichen planus is a chronic inflammatory skin condition characterized by purple, flat-topped, itchy papules, often affecting the wrists, ankles, and oral mucosa, whereas dermatographia is a physical urticaria marked by raised, red, and itchy wheals that appear after skin scratching or pressure. The etiology of lichen planus involves autoimmune mechanisms targeting basal keratinocytes, contrasting with dermatographia's hypersensitivity reaction to mechanical stimuli without an autoimmune component. Diagnosis of lichen planus relies on clinical examination and biopsy showing band-like lymphocytic infiltrate, while dermatographia is primarily diagnosed through patient history and a simple skin scratch test provoking a wheal-and-flare response.
Symptoms Comparison: Lichen Planus vs Dermatographia
Lichen planus presents with flat-topped, violaceous papules often accompanied by intense itching and mucosal lesions, while dermatographia features raised, red wheals resembling hives triggered by light skin scratching. The pruritus in lichen planus is persistent and may involve nails or scalp, causing hair loss, whereas dermatographia's itching and welting occur rapidly and resolve within 30 minutes. Both conditions exhibit skin inflammation, but lichen planus shows characteristic polygonal plaques with Wickham's striae, contrasting the transient linear urticaria seen in dermatographia.
Diagnosing Lichen Planus and Dermatographia
Diagnosing Lichen Planus involves identifying violaceous, flat-topped papules often with Wickham's striae through clinical examination and confirming with skin biopsy showing band-like lymphocytic infiltrate at the dermoepidermal junction. Dermatographia diagnosis is primarily clinical, characterized by wheal-and-flare responses elicited by gentle scratching, with no specific laboratory tests required. Differentiating between these conditions relies on visual assessment of lesion morphology, patient history, and histopathological evaluation for Lichen Planus versus the immediate skin reactivity seen in Dermatographia.
Risk Factors and Triggers for Each Condition
Lichen planus risk factors include genetic predisposition, hepatitis C virus infection, certain medications like beta-blockers, and autoimmune diseases. Dermatographia triggers involve mechanical skin irritation such as scratching, pressure, or tight clothing, with stress, heat, and allergies also exacerbating symptoms. Both conditions may worsen with immune system dysregulation, but lichen planus primarily involves inflammatory responses while dermatographia is characterized by physical urticaria.
Treatment Options for Lichen Planus
Lichen planus treatment primarily involves corticosteroids, either topical or systemic, to reduce inflammation and alleviate symptoms. Immunomodulatory agents such as calcineurin inhibitors and retinoids may be used in resistant cases, while phototherapy is an alternative approach for extensive lesions. Unlike dermatographia, which is managed by antihistamines to control histamine-induced skin reactions, lichen planus requires targeted immunosuppressive therapy to address its autoimmune nature.
Managing and Treating Dermatographia
Managing dermatographia involves avoiding triggers such as tight clothing and prolonged scratching to minimize skin irritation. Treatments primarily include antihistamines like cetirizine or hydroxyzine to reduce itching and histamine release. In severe cases, topical corticosteroids or immunomodulators may be prescribed to control inflammation and improve symptoms.
Prognosis and Long-Term Outlook
Lichen planus often has a chronic course with potential for spontaneous resolution within 1 to 2 years, but some cases may persist or recur, requiring long-term management due to risks of scarring and mucosal involvement. Dermatographia typically presents a benign, self-limiting condition with a favorable prognosis, as symptoms often diminish or resolve without lasting skin damage. Both conditions benefit from tailored treatment plans, yet lichen planus necessitates closer monitoring for complications like post-inflammatory pigmentation or secondary infections.
When to See a Dermatologist: Lichen Planus vs Dermatographia
Seek a dermatologist promptly if persistent purplish, flat-topped, itchy bumps characteristic of lichen planus develop, especially when accompanied by mucous membrane lesions or nail changes, as these may indicate a chronic inflammatory condition requiring specialized treatment. In contrast, dermatographia typically presents as raised, red linear welts triggered by skin pressure or scratching and usually resolves without extensive intervention; however, consultation is warranted if symptoms are severe or interfere with daily activities. Early diagnosis of lichen planus versus symptomatic management of dermatographia optimizes patient outcomes and prevents complications.
Lichen planus Infographic
 libterm.com
libterm.com