Anaphylaxis is a severe and potentially life-threatening allergic reaction requiring immediate medical attention. Symptoms can rapidly escalate, including difficulty breathing, swelling, and a sudden drop in blood pressure. Discover how to recognize early signs and manage this critical condition to protect your health by reading the full article.
Table of Comparison
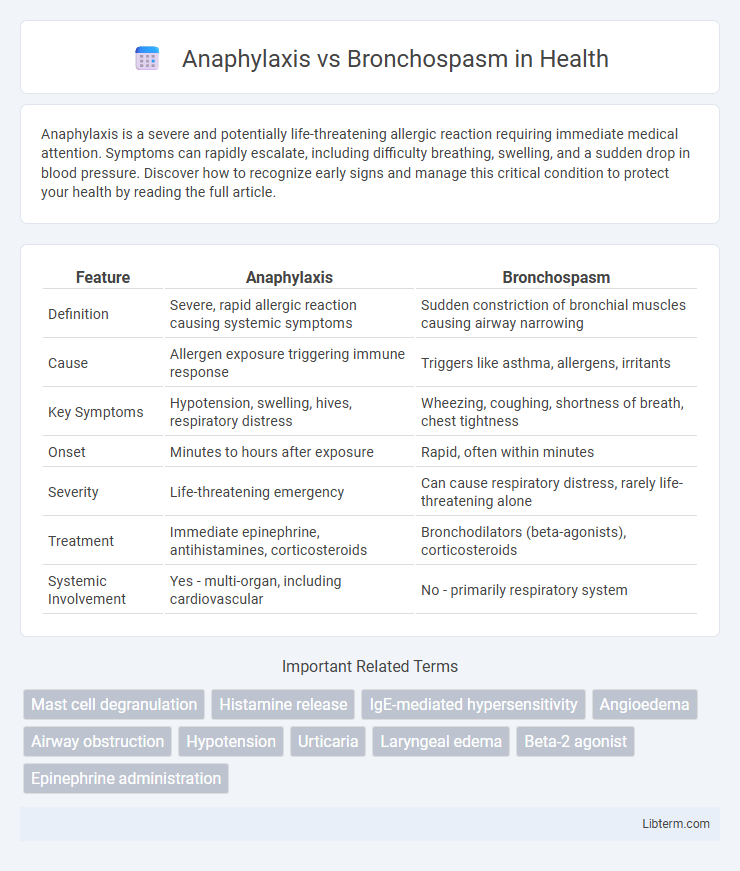
| Feature | Anaphylaxis | Bronchospasm |
|---|---|---|
| Definition | Severe, rapid allergic reaction causing systemic symptoms | Sudden constriction of bronchial muscles causing airway narrowing |
| Cause | Allergen exposure triggering immune response | Triggers like asthma, allergens, irritants |
| Key Symptoms | Hypotension, swelling, hives, respiratory distress | Wheezing, coughing, shortness of breath, chest tightness |
| Onset | Minutes to hours after exposure | Rapid, often within minutes |
| Severity | Life-threatening emergency | Can cause respiratory distress, rarely life-threatening alone |
| Treatment | Immediate epinephrine, antihistamines, corticosteroids | Bronchodilators (beta-agonists), corticosteroids |
| Systemic Involvement | Yes - multi-organ, including cardiovascular | No - primarily respiratory system |
Introduction to Anaphylaxis and Bronchospasm
Anaphylaxis is a severe, rapid-onset allergic reaction characterized by systemic vasodilation, airway edema, and hypotension, which can lead to life-threatening symptoms. Bronchospasm refers to the sudden constriction of bronchial smooth muscles, primarily causing airflow obstruction and respiratory distress, often seen in asthma or allergic reactions. Both conditions involve airway compromise but differ in their pathophysiology and urgency of management.
Definition and Overview
Anaphylaxis is a severe, rapid-onset allergic reaction characterized by systemic symptoms including hypotension, airway swelling, and rash, often requiring immediate treatment with epinephrine. Bronchospasm refers to the sudden constriction of bronchial smooth muscle resulting in airway narrowing, commonly associated with asthma or allergic triggers, leading to wheezing and difficulty breathing. Both conditions affect the respiratory system but differ in scope, with anaphylaxis involving multi-organ involvement and bronchospasm primarily impacting the lungs.
Causes and Triggers
Anaphylaxis is primarily triggered by allergens such as foods (peanuts, shellfish), insect stings, medications (penicillin, aspirin), and latex, causing a rapid systemic allergic reaction. Bronchospasm often results from asthma, chronic obstructive pulmonary disease (COPD), respiratory infections, or exposure to irritants like smoke, cold air, and exercise. Both conditions involve airway constriction but differ in origin, with anaphylaxis driven by an immunoglobulin E (IgE)-mediated hypersensitivity and bronchospasm linked to airway inflammation and hyperreactivity.
Pathophysiology: How Each Condition Develops
Anaphylaxis is a severe systemic hypersensitivity reaction triggered by rapid IgE-mediated release of histamine and other mediators from mast cells and basophils, causing widespread vasodilation, increased vascular permeability, and smooth muscle contraction. Bronchospasm results from the excessive contraction of bronchial smooth muscle due to airway hyperresponsiveness, often provoked by irritants, allergens, or inflammatory mediators like leukotrienes and acetylcholine acting on the respiratory tract. While anaphylaxis involves multi-organ systemic effects and circulatory collapse, bronchospasm primarily affects the lower airways, leading to airflow obstruction and respiratory distress.
Signs and Symptoms Comparison
Anaphylaxis manifests with widespread symptoms such as urticaria, angioedema, hypotension, and airway swelling, whereas bronchospasm primarily presents with wheezing, chest tightness, and dyspnea due to airway constriction. In anaphylaxis, rapid onset of systemic symptoms including cardiovascular collapse and gastrointestinal distress is common, while bronchospasm usually shows localized respiratory distress without systemic involvement. Both conditions may feature respiratory difficulty, but stridor and skin changes strongly indicate anaphylaxis over bronchospasm.
Diagnosis Criteria and Tools
Anaphylaxis diagnosis relies on rapid identification of multisystem symptoms such as skin rash, respiratory distress, and hypotension following allergen exposure, supported by clinical criteria from organizations like the World Allergy Organization. Bronchospasm diagnosis primarily involves detecting reversible airway obstruction through spirometry tests showing reduced FEV1 and peak expiratory flow rates, alongside clinical signs like wheezing and dyspnea. Diagnostic tools for anaphylaxis include serum tryptase levels and patient history, whereas bronchospasm assessment depends heavily on pulmonary function tests and response to bronchodilators.
Emergency Management and Treatment
Anaphylaxis requires immediate administration of intramuscular epinephrine as the first-line treatment, followed by airway management, supplemental oxygen, and intravenous fluids to stabilize blood pressure. Bronchospasm, commonly seen in asthma or COPD exacerbations, is treated with inhaled short-acting beta-agonists like albuterol, systemic corticosteroids, and oxygen therapy to relieve bronchoconstriction and improve ventilation. Both conditions demand rapid assessment, continuous monitoring of respiratory status, and prompt escalation of care in emergency settings to prevent respiratory failure.
Prognosis and Potential Complications
Anaphylaxis carries a high risk of rapid respiratory failure and cardiovascular collapse if not promptly treated, with potential complications including shock, hypoxic brain injury, and multi-organ failure. Bronchospasm, often a component of anaphylaxis or asthma, typically affects airway obstruction and gas exchange but rarely leads to systemic compromise unless severe or untreated. Early intervention with epinephrine significantly improves anaphylaxis prognosis, whereas bronchospasm management focuses on bronchodilators to prevent progression to respiratory distress.
Prevention Strategies
Effective prevention of anaphylaxis centers on strict allergen avoidance, use of medical alert identification, and carrying epinephrine auto-injectors for immediate treatment. Bronchospasm prevention focuses on identifying and managing triggers such as allergens, irritants, or exercise, alongside consistent use of prescribed bronchodilators and anti-inflammatory medications like inhaled corticosteroids. Both conditions benefit from personalized action plans and regular consultation with healthcare providers to optimize management and reduce risk.
Key Differences: Anaphylaxis vs Bronchospasm
Anaphylaxis is a severe systemic allergic reaction involving multiple organ systems, characterized by rapid onset of symptoms such as hypotension, urticaria, and airway obstruction. Bronchospasm specifically refers to the constriction of bronchial muscles causing wheezing and shortness of breath, often triggered by asthma or allergic reactions but without systemic involvement. Key differences include anaphylaxis's potential for widespread cardiovascular collapse versus bronchospasm's localized respiratory effect.
Anaphylaxis Infographic
 libterm.com
libterm.com