Pulmonary embolism occurs when a blood clot blocks an artery in the lungs, leading to severe respiratory issues and potentially life-threatening complications. Accurate diagnosis and prompt treatment are crucial to improving patient outcomes and preventing long-term damage. Discover more about the symptoms, risk factors, and treatment options to better understand how pulmonary embolism can affect your health.
Table of Comparison
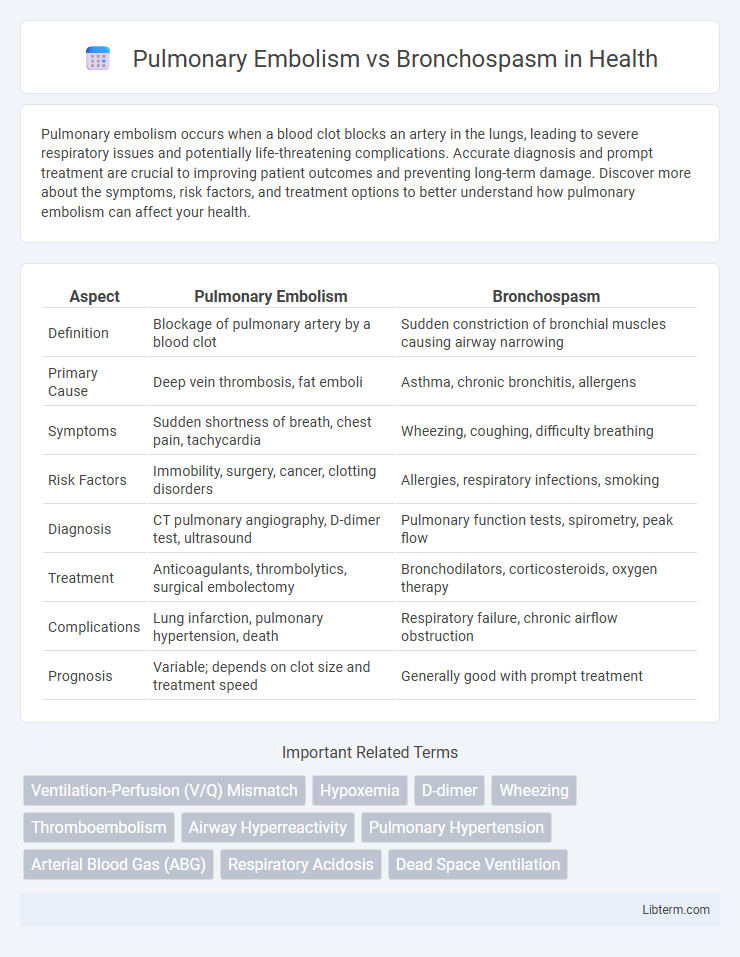
| Aspect | Pulmonary Embolism | Bronchospasm |
|---|---|---|
| Definition | Blockage of pulmonary artery by a blood clot | Sudden constriction of bronchial muscles causing airway narrowing |
| Primary Cause | Deep vein thrombosis, fat emboli | Asthma, chronic bronchitis, allergens |
| Symptoms | Sudden shortness of breath, chest pain, tachycardia | Wheezing, coughing, difficulty breathing |
| Risk Factors | Immobility, surgery, cancer, clotting disorders | Allergies, respiratory infections, smoking |
| Diagnosis | CT pulmonary angiography, D-dimer test, ultrasound | Pulmonary function tests, spirometry, peak flow |
| Treatment | Anticoagulants, thrombolytics, surgical embolectomy | Bronchodilators, corticosteroids, oxygen therapy |
| Complications | Lung infarction, pulmonary hypertension, death | Respiratory failure, chronic airflow obstruction |
| Prognosis | Variable; depends on clot size and treatment speed | Generally good with prompt treatment |
Introduction to Pulmonary Embolism and Bronchospasm
Pulmonary embolism (PE) is a life-threatening condition caused by a blockage in one of the pulmonary arteries, commonly due to blood clots originating in the deep veins of the legs or pelvis. Bronchospasm involves the sudden constriction of bronchial muscles, leading to airway narrowing and respiratory distress, often triggered by asthma, allergies, or chronic obstructive pulmonary disease (COPD). Differentiating PE from bronchospasm is critical for timely diagnosis and treatment since PE primarily affects vascular circulation while bronchospasm impacts airway patency.
Key Differences in Pathophysiology
Pulmonary embolism involves the sudden obstruction of pulmonary arteries by thromboemboli, leading to impaired blood flow and ventilation-perfusion mismatch, while bronchospasm is characterized by the constriction of bronchial smooth muscle causing airflow limitation primarily in the airways. The pathophysiology of pulmonary embolism centers on thrombus formation, vascular occlusion, and subsequent hypoxemia due to reduced pulmonary perfusion. In contrast, bronchospasm results from hyperreactivity of airway smooth muscles often triggered by allergens or irritants, causing reversible airway narrowing and increased airway resistance.
Common Causes and Risk Factors
Pulmonary embolism is primarily caused by deep vein thrombosis, with risk factors including prolonged immobility, recent surgery, and hypercoagulable states. Bronchospasm commonly results from asthma, chronic obstructive pulmonary disease (COPD), or exposure to allergens and irritants, with risk factors such as smoking, respiratory infections, and air pollution. Both conditions share some overlapping triggers like smoking but differ significantly in their underlying etiologies and pathophysiological mechanisms.
Typical Signs and Symptoms
Pulmonary embolism typically presents with sudden-onset dyspnea, pleuritic chest pain, tachycardia, and hypoxia, often accompanied by hemoptysis and unilateral leg swelling due to deep vein thrombosis. Bronchospasm usually manifests with wheezing, coughing, chest tightness, and shortness of breath, primarily associated with asthma or chronic obstructive pulmonary disease (COPD). While both conditions cause respiratory distress, hypoxemia is more severe in pulmonary embolism, and wheezing is a hallmark of bronchospasm.
Diagnostic Approaches and Tools
Pulmonary embolism diagnosis relies heavily on imaging techniques such as computed tomography pulmonary angiography (CTPA) and ventilation-perfusion (V/Q) scans, alongside D-dimer blood tests to assess clot presence. In contrast, bronchospasm evaluation prioritizes spirometry to measure airflow obstruction and peak expiratory flow rate (PEFR) monitoring, often supplemented by bronchoprovocation tests like methacholine challenge. Both conditions require thorough clinical assessment, but imaging is crucial for pulmonary embolism confirmation, whereas lung function tests dominate bronchospasm detection.
Clinical Presentation: Comparing the Onset
Pulmonary embolism typically presents with a sudden onset of symptoms such as acute dyspnea, pleuritic chest pain, and tachypnea, often following a triggering event like deep vein thrombosis or recent surgery. In contrast, bronchospasm usually develops more gradually, characterized by wheezing, coughing, and progressive shortness of breath, commonly seen in asthma or chronic obstructive pulmonary disease exacerbations. Recognizing the distinct timing and symptom patterns is crucial for accurate differential diagnosis and prompt management.
Treatment Strategies and Management
Treatment strategies for pulmonary embolism primarily involve anticoagulation therapy with agents such as heparin, warfarin, or direct oral anticoagulants to prevent clot propagation and reduce mortality risk. Management of bronchospasm centers on bronchodilators like short-acting beta-agonists (albuterol) and corticosteroids to relieve airway constriction and inflammation. In severe cases, pulmonary embolism may require thrombolytic therapy or surgical intervention, while refractory bronchospasm necessitates oxygen therapy or mechanical ventilation.
Prognosis and Complications
Pulmonary embolism carries a high risk of mortality and can lead to complications such as chronic thromboembolic pulmonary hypertension, right ventricular failure, and recurrent embolism if untreated. Bronchospasm generally has a better prognosis, with complications primarily related to airway obstruction, including respiratory distress and hypoxemia, especially in patients with underlying asthma or COPD. Early diagnosis and appropriate management are critical in both conditions to reduce morbidity and prevent long-term complications.
Prevention and Risk Reduction
Effective prevention of pulmonary embolism centers on early mobilization, use of anticoagulants, and compression stockings to reduce venous thromboembolism risk in hospitalized or immobile patients. Bronchospasm risk reduction emphasizes avoiding triggers such as allergens, irritants, and smoking, alongside adherence to prescribed inhaled corticosteroids and bronchodilators to control underlying airway inflammation. Identifying patient-specific risk factors, including thrombophilia for embolism and asthma or COPD for bronchospasm, is critical to tailoring prevention strategies.
When to Seek Emergency Care
Seek emergency care immediately if sudden shortness of breath, chest pain, rapid heartbeat, or coughing up blood occurs, as these symptoms indicate a possible pulmonary embolism requiring urgent medical attention. Bronchospasm symptoms, such as wheezing, difficulty breathing, and persistent coughing, necessitate emergency care if they worsen despite using prescribed inhalers or if oxygen levels drop significantly. Prompt evaluation and treatment in an emergency setting reduce risks of complications for both pulmonary embolism and severe bronchospasm episodes.
Pulmonary Embolism Infographic
 libterm.com
libterm.com