Interstitial nephritis is an inflammation of the kidney's interstitial tissue often caused by infections, medications, or autoimmune diseases, leading to impaired kidney function. Symptoms can include fever, rash, and decreased urine output, and early diagnosis is crucial to prevent long-term damage. Discover more about the causes, symptoms, and treatment options to protect your kidney health by reading the rest of the article.
Table of Comparison
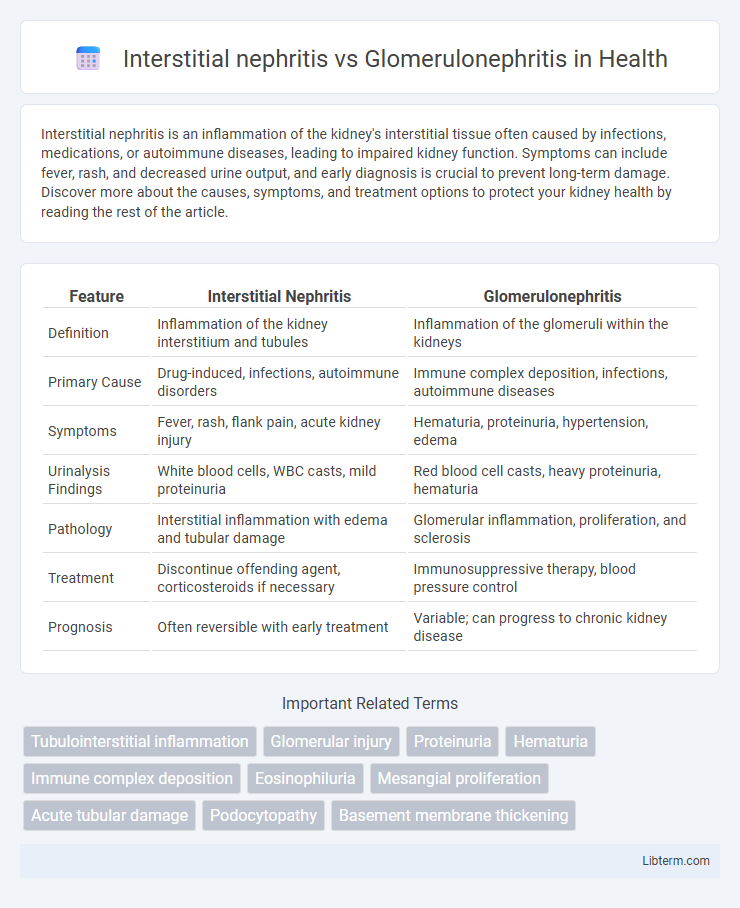
| Feature | Interstitial Nephritis | Glomerulonephritis |
|---|---|---|
| Definition | Inflammation of the kidney interstitium and tubules | Inflammation of the glomeruli within the kidneys |
| Primary Cause | Drug-induced, infections, autoimmune disorders | Immune complex deposition, infections, autoimmune diseases |
| Symptoms | Fever, rash, flank pain, acute kidney injury | Hematuria, proteinuria, hypertension, edema |
| Urinalysis Findings | White blood cells, WBC casts, mild proteinuria | Red blood cell casts, heavy proteinuria, hematuria |
| Pathology | Interstitial inflammation with edema and tubular damage | Glomerular inflammation, proliferation, and sclerosis |
| Treatment | Discontinue offending agent, corticosteroids if necessary | Immunosuppressive therapy, blood pressure control |
| Prognosis | Often reversible with early treatment | Variable; can progress to chronic kidney disease |
Overview: Interstitial Nephritis vs Glomerulonephritis
Interstitial nephritis primarily affects the renal interstitium and tubules, leading to inflammation that disrupts kidney function and often results from allergic reactions or infections. In contrast, glomerulonephritis involves immune-mediated inflammation targeting the glomeruli, causing impaired filtration and proteinuria. Both conditions can lead to acute or chronic kidney disease but differ significantly in their pathophysiology, clinical presentation, and treatment approaches.
Definitions and Core Differences
Interstitial nephritis is characterized by inflammation of the kidney's interstitial tissue, primarily affecting the spaces between renal tubules, often due to drug reactions or infections. Glomerulonephritis involves inflammation of the glomeruli, the kidney's filtering units, leading to impaired filtration and possible blood or protein in the urine. The core difference lies in the anatomical location affected: interstitial nephritis targets the interstitium and tubules, while glomerulonephritis targets the glomeruli, resulting in distinct clinical presentations and pathological processes.
Etiology and Risk Factors
Interstitial nephritis primarily arises from allergic reactions to medications such as NSAIDs, antibiotics, and diuretics, as well as infections and autoimmune diseases like Sjogren's syndrome. Glomerulonephritis is most commonly caused by post-infectious immune responses, systemic conditions like lupus erythematosus, and chronic diseases including diabetes mellitus and hypertension. Both conditions are influenced by risk factors including genetic predisposition, existing autoimmune disorders, and exposure to nephrotoxic agents.
Pathophysiology: Mechanisms of Kidney Injury
Interstitial nephritis involves inflammation primarily affecting the renal interstitium and tubules, often triggered by hypersensitivity reactions or infections, leading to tubular cell injury and edema. Glomerulonephritis, however, is characterized by immune-mediated damage to the glomeruli, causing capillary wall inflammation, disruption of the glomerular filtration barrier, and proteinuria. Both conditions result in impaired kidney function, but differ in the primary site of injury and underlying immunopathological mechanisms.
Clinical Manifestations and Symptoms
Interstitial nephritis presents with symptoms such as fever, rash, eosinophilia, and flank pain, often accompanied by signs of acute kidney injury like elevated serum creatinine and pyuria without significant proteinuria. Glomerulonephritis typically manifests with hematuria, proteinuria, hypertension, and edema, reflecting glomerular inflammation and impaired filtration. Both conditions may cause renal dysfunction, but the presence of systemic allergic symptoms and prominent urinary eosinophils favors interstitial nephritis, whereas nephritic syndrome features suggest glomerulonephritis.
Laboratory Findings and Urinalysis
Interstitial nephritis typically presents with eosinophilia and sterile pyuria, while urinalysis often reveals white blood cell casts and mild proteinuria. In contrast, glomerulonephritis shows elevated serum creatinine and blood urea nitrogen (BUN) with significant proteinuria, hematuria, and red blood cell casts in the urine. Serologic markers such as anti-GBM antibodies or ANCA are more commonly associated with glomerulonephritis, aiding in differentiation from interstitial nephritis.
Diagnostic Approaches and Imaging
Diagnostic approaches for interstitial nephritis primarily involve urinalysis revealing sterile pyuria, eosinophiluria, and mild proteinuria, with renal biopsy showing interstitial inflammation. In contrast, glomerulonephritis diagnosis relies on serologic tests like anti-GBM antibodies, ANCA, and complement levels, with urinalysis indicating hematuria and red blood cell casts, and biopsy revealing glomerular injury. Imaging modalities such as renal ultrasound are often nonspecific but can show normal or enlarged kidneys in interstitial nephritis, while glomerulonephritis may demonstrate normal size or chronic changes; advanced imaging like MRI or CT is rarely diagnostic but aids in excluding other conditions.
Treatment Strategies and Management
Treatment strategies for interstitial nephritis primarily involve discontinuing the offending drug or addressing the underlying infection, with corticosteroids often prescribed to reduce inflammation. Management of glomerulonephritis focuses on controlling blood pressure using ACE inhibitors or ARBs, immunosuppressive therapy to limit immune-mediated damage, and supportive measures like diuretics and dietary modifications. Both conditions require close monitoring of renal function and electrolyte levels to prevent progression to chronic kidney disease.
Prognosis and Long-term Outcomes
Interstitial nephritis often has a better prognosis with potential for renal function recovery if the underlying cause is promptly addressed, while glomerulonephritis may lead to chronic kidney disease or end-stage renal failure depending on the severity and type. Long-term outcomes in interstitial nephritis depend on the extent of fibrosis and ongoing exposure to causative agents, whereas glomerulonephritis prognosis is influenced by the degree of glomerular damage and response to immunosuppressive therapy. Both conditions require careful monitoring of renal function and management to prevent irreversible kidney damage.
Key Points: Comparing Interstitial Nephritis and Glomerulonephritis
Interstitial nephritis primarily involves inflammation of the kidney interstitium and tubules, often caused by allergic reactions or infections, whereas glomerulonephritis targets the glomeruli, frequently resulting from autoimmune disorders or infections. Symptoms of interstitial nephritis include fever, rash, and eosinophilia, while glomerulonephritis typically presents with hematuria, proteinuria, and hypertension. Diagnosis relies on kidney biopsy and laboratory tests showing distinct histopathologic findings, with treatment strategies tailored to the underlying cause and extent of renal involvement.
Interstitial nephritis Infographic
 libterm.com
libterm.com