Pyuria is characterized by the presence of excess white blood cells in the urine, often indicating a urinary tract infection or inflammation. This condition can cause symptoms such as cloudy urine, discomfort during urination, and frequent urges to urinate. Discover how to recognize, diagnose, and effectively manage pyuria by reading the full article.
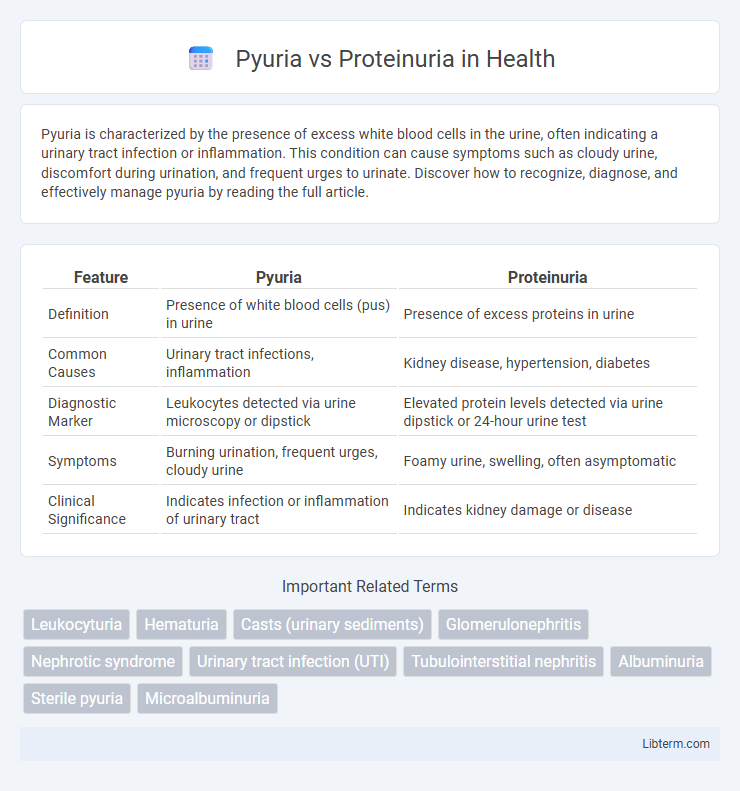
Table of Comparison
| Feature | Pyuria | Proteinuria |
|---|---|---|
| Definition | Presence of white blood cells (pus) in urine | Presence of excess proteins in urine |
| Common Causes | Urinary tract infections, inflammation | Kidney disease, hypertension, diabetes |
| Diagnostic Marker | Leukocytes detected via urine microscopy or dipstick | Elevated protein levels detected via urine dipstick or 24-hour urine test |
| Symptoms | Burning urination, frequent urges, cloudy urine | Foamy urine, swelling, often asymptomatic |
| Clinical Significance | Indicates infection or inflammation of urinary tract | Indicates kidney damage or disease |
Understanding Pyuria: Definition and Causes
Pyuria is characterized by the presence of an elevated number of white blood cells (WBCs) in the urine, typically indicating a urinary tract infection, inflammation, or kidney disorders. Common causes of pyuria include bacterial infections such as cystitis, pyelonephritis, and sexually transmitted infections, as well as non-infectious conditions like interstitial nephritis or urinary tract stones. Differentiating pyuria from proteinuria, which involves excess protein in the urine and often signals kidney damage, is crucial for accurate diagnosis and treatment.
Proteinuria Explained: Key Facts and Origins
Proteinuria refers to the presence of excess proteins, primarily albumin, in the urine, indicating potential kidney damage or disease. It often originates from glomerular injury, increased tubular protein reabsorption failure, or systemic conditions such as diabetes and hypertension. Persistent proteinuria requires thorough evaluation to assess renal function and prevent progression to chronic kidney disease.
Pathophysiology: How Pyuria and Proteinuria Develop
Pyuria develops due to the infiltration of white blood cells into the urine, typically triggered by infection or inflammation in the urinary tract, causing leukocytes to accumulate and indicate immune response. Proteinuria occurs when the glomerular filtration barrier in the kidneys is damaged or compromised, allowing abnormal amounts of plasma proteins, mainly albumin, to leak into the urine. Both conditions reflect underlying pathophysiological changes: pyuria indicates an active immune or infectious process, whereas proteinuria signifies structural or functional impairment of the glomerular filtration unit.
Common Symptoms: Pyuria vs Proteinuria
Pyuria commonly presents with symptoms such as cloudy or foul-smelling urine, dysuria, and increased frequency or urgency of urination, indicative of urinary tract infections or inflammation. Proteinuria often remains asymptomatic but may be associated with foamy urine and signs of underlying kidney disease, including swelling in extremities and fatigue. Both conditions reflect different pathological processes, with pyuria signaling infection or inflammation and proteinuria pointing to renal damage or dysfunction.
Diagnostic Approaches: Differentiating the Two
Diagnostic approaches to differentiate pyuria and proteinuria primarily involve microscopic urinalysis and biochemical testing. Pyuria is identified by the presence of white blood cells (WBCs) in urine, typically detected through urine microscopy or dipstick leukocyte esterase testing, indicating urinary tract infection or inflammation. Proteinuria is confirmed by quantifying protein levels using urine protein-to-creatinine ratio or 24-hour urine protein collection, distinguishing it from pyuria and suggesting glomerular or tubular kidney disease.
Underlying Diseases: Associated Conditions
Pyuria commonly indicates urinary tract infections, kidney inflammation such as pyelonephritis, or interstitial nephritis, often caused by bacterial infections or autoimmune disorders. Proteinuria is primarily associated with glomerular diseases including diabetic nephropathy, hypertensive nephrosclerosis, and glomerulonephritis, reflecting increased permeability of the glomerular basement membrane. Both conditions can coexist in systemic diseases like lupus erythematosus, where inflammation and kidney damage contribute to urinary abnormalities.
Risk Factors for Pyuria and Proteinuria
Pyuria commonly results from urinary tract infections, kidney inflammation, or systemic conditions like diabetes and immunosuppression, which increase susceptibility to bacterial invasion or inflammatory processes in the urinary tract. Proteinuria risk factors include diabetes mellitus, hypertension, glomerulonephritis, and chronic kidney disease that lead to glomerular damage and increased protein leakage into the urine. Both conditions are often linked to underlying renal pathology, with pyuria indicating infection or inflammation and proteinuria signaling glomerular filtration barrier dysfunction.
Laboratory Findings and Interpretation
Pyuria is characterized by the presence of elevated white blood cells (WBCs) in the urine, typically greater than 10 WBCs per high power field, indicating inflammation or infection in the urinary tract. Proteinuria is defined by abnormal amounts of protein in the urine, often measured by urine dipstick tests or 24-hour urine protein collection, with levels exceeding 150 mg/day considered abnormal. Laboratory interpretation distinguishes pyuria as a marker of urinary tract infections or renal inflammation, while proteinuria signals glomerular or tubular damage, requiring specific diagnostic evaluation.
Treatment Strategies: Management of Each Condition
Treatment strategies for pyuria primarily involve addressing the underlying infection with appropriate antibiotics, guided by urine culture results, alongside supportive measures such as hydration and pain management. Management of proteinuria focuses on controlling the underlying cause, often through the use of angiotensin-converting enzyme inhibitors (ACE inhibitors) or angiotensin receptor blockers (ARBs) to reduce protein excretion and protect kidney function. Monitoring patient response through regular urine tests and kidney function assessments is essential to tailor treatment plans for both conditions effectively.
Prognosis and Clinical Outcomes Comparison
Pyuria indicates inflammation or infection in the urinary tract and often predicts favorable outcomes with appropriate antibiotic treatment, although persistent pyuria may signal chronic urinary tract conditions or underlying systemic diseases. Proteinuria reflects kidney damage or dysfunction and is a critical prognostic factor for chronic kidney disease progression, cardiovascular morbidity, and increased mortality risk. Clinical outcomes differ as pyuria generally resolves with infection control, whereas proteinuria requires long-term management to prevent renal failure and adverse systemic effects.
Pyuria Infographic
 libterm.com
libterm.com