Meningitis is a serious infection causing inflammation of the protective membranes covering the brain and spinal cord, leading to symptoms like severe headache, fever, and neck stiffness. Early detection and treatment are crucial to prevent long-term complications or fatal outcomes. Discover essential facts and prevention tips to protect your health by reading the rest of the article.
Table of Comparison
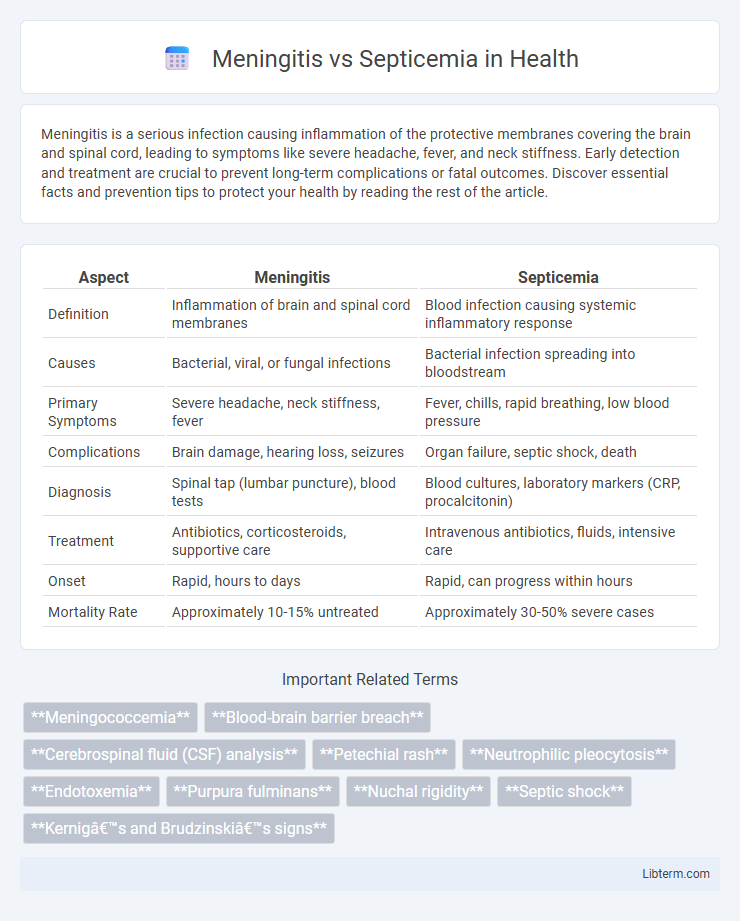
| Aspect | Meningitis | Septicemia |
|---|---|---|
| Definition | Inflammation of brain and spinal cord membranes | Blood infection causing systemic inflammatory response |
| Causes | Bacterial, viral, or fungal infections | Bacterial infection spreading into bloodstream |
| Primary Symptoms | Severe headache, neck stiffness, fever | Fever, chills, rapid breathing, low blood pressure |
| Complications | Brain damage, hearing loss, seizures | Organ failure, septic shock, death |
| Diagnosis | Spinal tap (lumbar puncture), blood tests | Blood cultures, laboratory markers (CRP, procalcitonin) |
| Treatment | Antibiotics, corticosteroids, supportive care | Intravenous antibiotics, fluids, intensive care |
| Onset | Rapid, hours to days | Rapid, can progress within hours |
| Mortality Rate | Approximately 10-15% untreated | Approximately 30-50% severe cases |
Understanding Meningitis and Septicemia
Meningitis is an inflammation of the protective membranes covering the brain and spinal cord, typically caused by bacterial, viral, or fungal infections, while septicemia refers to a systemic bloodstream infection characterized by the presence of harmful bacteria and toxins. Both conditions can result in severe complications such as organ failure and require prompt medical intervention, but meningitis primarily affects the central nervous system, whereas septicemia impacts the entire body through blood infection. Early diagnosis through laboratory testing and clinical evaluation is critical to differentiate between meningitis and septicemia for effective treatment and improved patient outcomes.
Causes and Risk Factors
Meningitis is primarily caused by viral or bacterial infections, with Streptococcus pneumoniae and Neisseria meningitidis being the most common bacterial agents, while septicemia results from bacteria entering the bloodstream, often due to infections in the lungs, urinary tract, or skin. Risk factors for meningitis include age under five, weakened immune system, close living conditions, and lack of vaccination, whereas septicemia risk factors encompass chronic illnesses, invasive medical procedures, and compromised immunity. Both conditions share bacterial infections as a common cause but differ in their primary sites of infection and the pathways through which they affect the body.
Key Differences Between Meningitis and Septicemia
Meningitis primarily involves inflammation of the meninges surrounding the brain and spinal cord, often triggered by bacterial or viral infections, whereas septicemia is a systemic bloodstream infection causing widespread inflammation and sepsis. Key differences include meningitis presenting with symptoms like severe headache, neck stiffness, and photophobia, while septicemia manifests as fever, chills, rapid breathing, and potential organ failure. Diagnosis involves cerebrospinal fluid analysis for meningitis and blood cultures for septicemia, guiding distinct treatment approaches typically involving targeted antibiotics and supportive care.
Signs and Symptoms Comparison
Meningitis presents with symptoms such as severe headache, neck stiffness, fever, sensitivity to light, and confusion, often accompanied by nausea and vomiting. Septicemia, also known as blood poisoning, typically causes high fever, chills, rapid breathing, and a distinctive rash, along with low blood pressure and organ dysfunction indicating systemic infection. Both conditions can cause fever and fatigue, but the presence of neck stiffness and neurological signs are more specific to meningitis, whereas septicemia's hallmark is widespread infection leading to sepsis and shock.
How Meningitis Develops
Meningitis develops when bacterial, viral, or fungal infections invade the protective membranes (meninges) surrounding the brain and spinal cord, causing inflammation. This condition often begins after pathogens enter the bloodstream through respiratory tract infections or wounds, enabling them to breach the blood-brain barrier. In contrast to septicemia, which is the presence of bacteria in the bloodstream causing systemic infection, meningitis specifically targets the central nervous system, leading to symptoms such as severe headache, neck stiffness, and altered mental status.
How Septicemia Progresses
Septicemia, also known as blood poisoning, progresses rapidly as bacteria enter the bloodstream, triggering a systemic inflammatory response that can lead to septic shock and multiple organ failure. Unlike meningitis, which specifically affects the protective membranes of the brain and spinal cord, septicemia spreads infection throughout the body, causing widespread tissue damage and severe complications. Early detection and aggressive antibiotic treatment are crucial to prevent the progression of septicemia to life-threatening stages.
Diagnostic Methods for Each Condition
Meningitis is diagnosed primarily through cerebrospinal fluid analysis obtained via lumbar puncture, including cell count, glucose, protein levels, and bacterial cultures; PCR testing further identifies viral or bacterial pathogens. Septicemia diagnosis relies on blood cultures to detect bloodstream infections, alongside complete blood count (CBC), lactate levels, and biomarkers like procalcitonin to assess systemic inflammation. Imaging studies and clinical signs complement laboratory tests for accurate differentiation and timely treatment of these critical conditions.
Treatment Options and Approaches
Treatment options for meningitis typically involve high-dose intravenous antibiotics such as ceftriaxone or vancomycin administered promptly to target bacterial infection, alongside corticosteroids like dexamethasone to reduce inflammation and prevent neurological complications. Septicemia treatment emphasizes aggressive intravenous fluids to maintain blood pressure, broad-spectrum antibiotics adjusted based on culture results, and supportive measures including vasopressors and oxygen therapy to manage systemic organ dysfunction. Both conditions require intensive monitoring in hospital settings, with meningitis focusing on neuroprotective strategies and septicemia on stabilizing hemodynamics and preventing multi-organ failure.
Complications and Long-term Effects
Meningitis often leads to complications such as brain damage, hearing loss, and learning disabilities, while septicemia can cause widespread organ failure, septic shock, and amputation due to tissue necrosis. Long-term effects of meningitis include cognitive impairments and seizures, whereas survivors of septicemia may experience chronic fatigue, post-traumatic stress disorder, and impaired organ function. Both conditions require prompt treatment to reduce the risk of severe, lasting health impacts.
Prevention and Vaccination Strategies
Prevention of meningitis and septicemia relies heavily on timely vaccination, with vaccines like the meningococcal, pneumococcal, and Haemophilus influenzae type b (Hib) effectively reducing the incidence of both infections. Proper hygiene practices, including regular handwashing and avoiding close contact with infected individuals, also play a critical role in preventing the spread of pathogens responsible for these diseases. Public health strategies emphasize early immunization schedules and outbreak control measures to minimize the burden of meningitis and septicemia globally.
Meningitis Infographic
 libterm.com
libterm.com