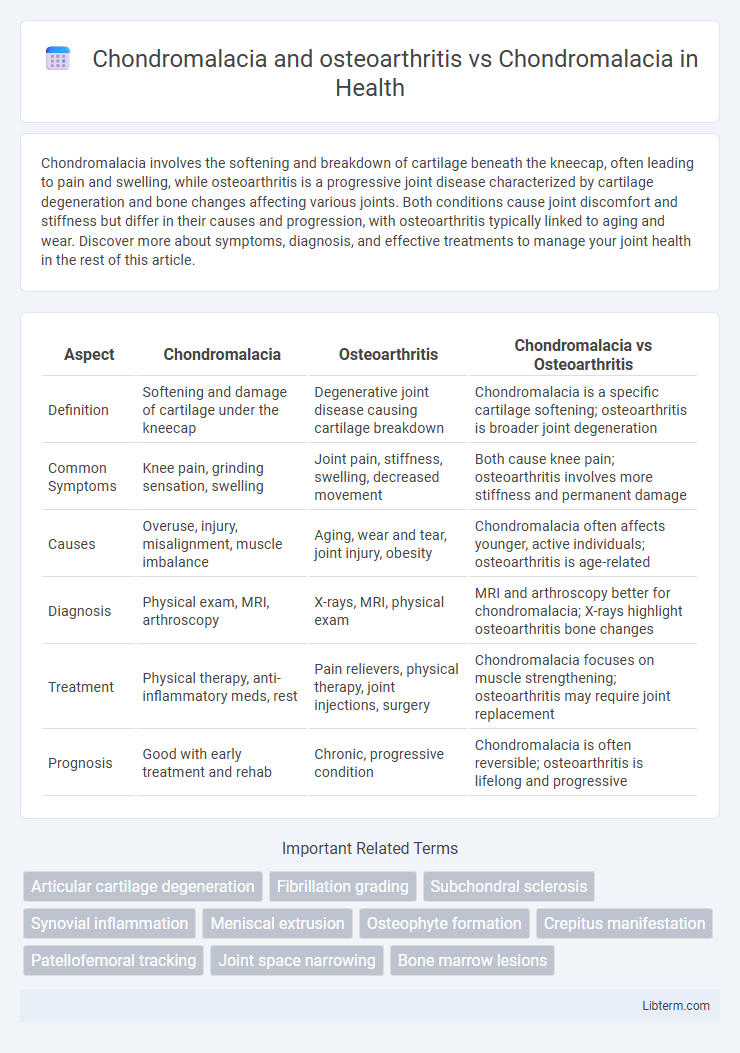
Chondromalacia involves the softening and breakdown of cartilage beneath the kneecap, often leading to pain and swelling, while osteoarthritis is a progressive joint disease characterized by cartilage degeneration and bone changes affecting various joints. Both conditions cause joint discomfort and stiffness but differ in their causes and progression, with osteoarthritis typically linked to aging and wear. Discover more about symptoms, diagnosis, and effective treatments to manage your joint health in the rest of this article.
Table of Comparison
| Aspect | Chondromalacia | Osteoarthritis | Chondromalacia vs Osteoarthritis |
|---|---|---|---|
| Definition | Softening and damage of cartilage under the kneecap | Degenerative joint disease causing cartilage breakdown | Chondromalacia is a specific cartilage softening; osteoarthritis is broader joint degeneration |
| Common Symptoms | Knee pain, grinding sensation, swelling | Joint pain, stiffness, swelling, decreased movement | Both cause knee pain; osteoarthritis involves more stiffness and permanent damage |
| Causes | Overuse, injury, misalignment, muscle imbalance | Aging, wear and tear, joint injury, obesity | Chondromalacia often affects younger, active individuals; osteoarthritis is age-related |
| Diagnosis | Physical exam, MRI, arthroscopy | X-rays, MRI, physical exam | MRI and arthroscopy better for chondromalacia; X-rays highlight osteoarthritis bone changes |
| Treatment | Physical therapy, anti-inflammatory meds, rest | Pain relievers, physical therapy, joint injections, surgery | Chondromalacia focuses on muscle strengthening; osteoarthritis may require joint replacement |
| Prognosis | Good with early treatment and rehab | Chronic, progressive condition | Chondromalacia is often reversible; osteoarthritis is lifelong and progressive |
Understanding Chondromalacia: Causes and Symptoms
Chondromalacia involves the softening and deterioration of cartilage beneath the kneecap, often caused by repetitive stress, injury, or misalignment, leading to knee pain and swelling. Osteoarthritis, a degenerative joint disease, progresses as cartilage breaks down and bone changes occur, typically resulting in joint stiffness and reduced mobility. Differentiating chondromalacia from osteoarthritis is crucial, as early diagnosis of cartilage damage in chondromalacia can prevent progression to more severe joint conditions.
What is Osteoarthritis? Key Features Explained
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage, leading to pain, stiffness, and reduced mobility, often affecting weight-bearing joints like knees and hips. Chondromalacia, specifically referring to softening or damage of the cartilage under the kneecap, is often an early sign of cartilage deterioration but not as advanced as osteoarthritis. Key features of osteoarthritis include joint space narrowing, bone spurs, and chronic inflammation, distinguishing it from chondromalacia, which primarily involves cartilage softening without significant bone changes.
Chondromalacia vs Osteoarthritis: Core Differences
Chondromalacia involves the softening and early degradation of cartilage, primarily affecting the knee's patellar surface, often resulting from overuse or injury. Osteoarthritis represents a more advanced, degenerative joint disease characterized by cartilage erosion, bone remodeling, and joint inflammation, commonly impacting multiple joints such as knees, hips, and hands. Core differences include Chondromalacia's localized cartilage softening versus Osteoarthritis's progressive joint deterioration accompanied by bone changes and chronic pain.
Risk Factors for Chondromalacia and Osteoarthritis
Chondromalacia and osteoarthritis share common risk factors such as age, joint overuse, and injury, which contribute to cartilage degeneration and joint inflammation. Obesity significantly increases the mechanical load on joints, exacerbating cartilage breakdown in both conditions. Genetics, joint alignment abnormalities, and repetitive stress play crucial roles in the development and progression of chondromalacia and osteoarthritis.
Similarities in Joint Damage and Cartilage Wear
Chondromalacia and osteoarthritis both involve the deterioration of articular cartilage, leading to joint pain and reduced mobility, primarily affecting weight-bearing joints such as the knees. Both conditions exhibit cartilage softening, fibrillation, and progressive erosion, which compromise joint function and contribute to inflammation. The shared pathological hallmark is the degradation of cartilage matrix components like collagen and proteoglycans, causing similar patterns of joint damage despite differing etiologies.
Diagnosis: Differentiating Chondromalacia from Osteoarthritis
Diagnosis of chondromalacia involves MRI and arthroscopy to assess cartilage softening and damage, while osteoarthritis diagnosis focuses on X-rays revealing joint space narrowing and bone spurs. Chondromalacia primarily affects the patellar cartilage, causing localized anterior knee pain, whereas osteoarthritis damages multiple joint components with more widespread symptoms. Differentiating these conditions relies on detailed imaging and clinical evaluation of symptom patterns and cartilage integrity.
Treatment Strategies: Chondromalacia vs Osteoarthritis
Treatment strategies for chondromalacia primarily focus on reducing knee pain and inflammation through physical therapy, activity modification, and nonsteroidal anti-inflammatory drugs (NSAIDs), with emphasis on strengthening the quadriceps to improve patellar tracking. Osteoarthritis treatment extends beyond symptom management to include weight loss, joint injections such as corticosteroids or hyaluronic acid, and in severe cases, surgical interventions like total knee replacement to address joint degeneration. Both conditions benefit from early diagnosis, but osteoarthritis often requires a more comprehensive, multidisciplinary approach due to its progressive nature.
Preventive Measures for Joint Health
Chondromalacia and osteoarthritis both involve cartilage degradation, with osteoarthritis representing a more advanced joint condition characterized by cartilage loss and bone changes. Preventive measures for joint health include maintaining a healthy weight to reduce stress on joints, engaging in low-impact exercises such as swimming or cycling to strengthen muscles around the joints, and ensuring proper nutrition rich in omega-3 fatty acids and antioxidants for cartilage support. Early intervention through physical therapy and avoiding repetitive joint strain can help slow the progression of chondromalacia and delay the onset of osteoarthritis.
Prognosis and Long-Term Outlook
Chondromalacia primarily involves cartilage softening and is often reversible with proper physical therapy, whereas osteoarthritis represents a progressive joint degeneration with cartilage loss, leading to chronic pain and reduced mobility. The prognosis for chondromalacia is generally favorable if addressed early, while osteoarthritis typically involves a long-term decline requiring ongoing management and potential joint replacement. Long-term outlook for osteoarthritis includes increased disability risk, whereas chondromalacia patients maintain better joint function when treated promptly.
Frequently Asked Questions about Chondromalacia and Osteoarthritis
Chondromalacia involves the softening and breakdown of cartilage, primarily affecting the knee joint, whereas osteoarthritis results in the gradual degeneration of cartilage accompanied by bone changes and joint inflammation. Frequently asked questions about these conditions often center on symptoms like joint pain, stiffness, and reduced mobility, diagnostic methods including MRI and X-rays, and treatment options ranging from physical therapy to surgical interventions. Understanding the differences and overlapping features helps patients and clinicians tailor management plans to effectively address pain and improve joint function.
Chondromalacia and osteoarthritis Infographic
 libterm.com
libterm.com