Efficacy measures the ability of a treatment, intervention, or product to produce the desired beneficial effect under ideal conditions. Understanding efficacy helps determine how well a solution meets its intended purpose before widespread implementation. Explore the rest of this article to learn how efficacy impacts your choices and outcomes.
Table of Comparison
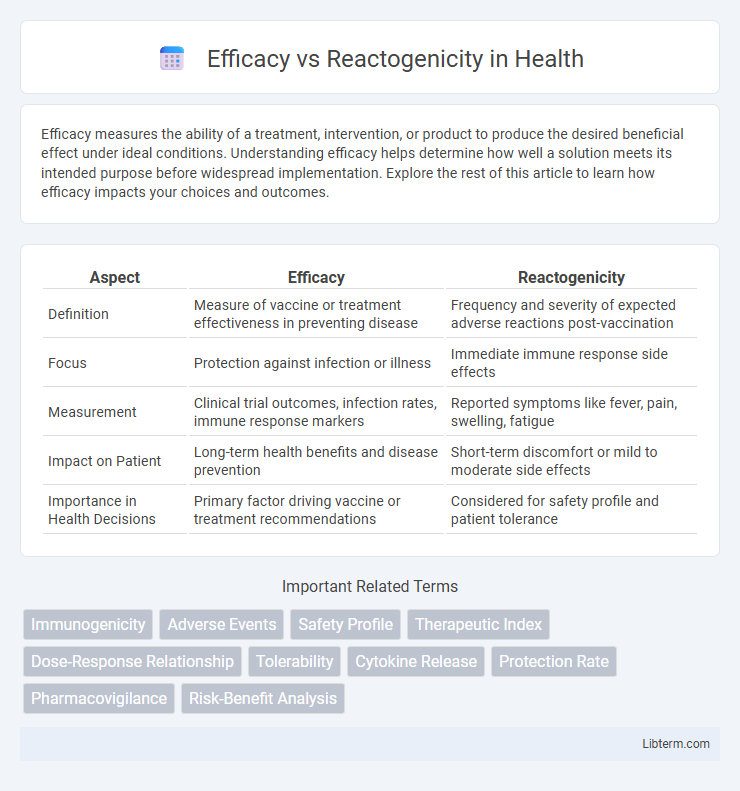
| Aspect | Efficacy | Reactogenicity |
|---|---|---|
| Definition | Measure of vaccine or treatment effectiveness in preventing disease | Frequency and severity of expected adverse reactions post-vaccination |
| Focus | Protection against infection or illness | Immediate immune response side effects |
| Measurement | Clinical trial outcomes, infection rates, immune response markers | Reported symptoms like fever, pain, swelling, fatigue |
| Impact on Patient | Long-term health benefits and disease prevention | Short-term discomfort or mild to moderate side effects |
| Importance in Health Decisions | Primary factor driving vaccine or treatment recommendations | Considered for safety profile and patient tolerance |
Introduction to Efficacy and Reactogenicity
Efficacy measures a vaccine's ability to prevent disease under controlled clinical trial conditions, reflecting its protective effect in reducing infection rates or severity. Reactogenicity refers to the short-term, expected immune responses and side effects following vaccination, such as pain at the injection site, fever, or fatigue, indicating the vaccine's stimulation of the immune system. Understanding both efficacy and reactogenicity is critical for evaluating a vaccine's overall benefit-risk profile and guiding public health vaccination strategies.
Defining Efficacy: What Does It Mean?
Efficacy measures the ability of a vaccine or treatment to produce the desired immune response or protection against a disease in controlled clinical trials. It quantifies the reduction in incidence of infection or symptoms among vaccinated individuals compared to unvaccinated controls. High efficacy indicates strong protective benefits, while balancing reactogenicity--short-term side effects--is crucial for overall vaccine performance and public acceptance.
Understanding Reactogenicity: Key Concepts
Reactogenicity refers to the physical reactions and side effects experienced after vaccination, such as pain, swelling, or fever, indicating the body's immune response activation. Understanding reactogenicity helps differentiate common, transient vaccine responses from rare adverse events, guiding vaccine safety assessments. Balancing reactogenicity with vaccine efficacy ensures optimized immunization strategies that maximize protection while minimizing discomfort.
Measuring Efficacy in Clinical Trials
Measuring efficacy in clinical trials involves assessing the vaccine's ability to prevent disease under controlled conditions by comparing infection rates between vaccinated and placebo groups. Clinical endpoints such as symptom reduction, confirmed infection cases, and immune response markers like antibody titers are critical for determining effectiveness. Rigorous data collection and statistical analysis ensure accurate differentiation between vaccine-induced protection and reactogenicity-related side effects.
Assessing Reactogenicity: Common Indicators
Assessing reactogenicity involves monitoring common indicators such as injection site pain, redness, swelling, and systemic symptoms like fever, fatigue, and headache. These signs provide critical data on the immune response intensity and potential tolerability of vaccines or treatments. Accurate measurement of reactogenicity helps balance efficacy with safety profiles essential for regulatory approval and public acceptance.
Factors Influencing Vaccine Efficacy
Vaccine efficacy is influenced by factors such as the genetic variability of the pathogen, host immune response diversity, and the vaccine formulation, including antigen choice and adjuvant presence. Reactogenicity, which refers to the physical manifestations of the immune response, can affect vaccine acceptance but does not directly correlate with efficacy levels. Environmental factors like storage conditions, administration route, and dosing schedule also play critical roles in optimizing vaccine efficacy.
Variables Affecting Reactogenicity Rates
Reactogenicity rates are influenced by variables such as age, vaccine type, and dosing interval, which modulate the intensity of adverse reactions post-vaccination. Younger individuals often experience higher reactogenicity due to more robust immune responses, while inactivated vaccines typically show lower reactogenicity compared to mRNA or viral vector vaccines. Vaccine formulation components, such as adjuvants, and recipients' prior exposure to antigens also significantly affect reactogenicity outcomes.
Balancing Efficacy and Reactogenicity in Public Health
Balancing efficacy and reactogenicity is crucial in vaccine development to ensure maximum public health benefits while minimizing adverse reactions. High vaccine efficacy reduces disease transmission and severity, but an increase in reactogenicity may lead to lower vaccine acceptance and compliance. Public health strategies must optimize this balance by selecting formulations that provide robust immunity with acceptable tolerability to achieve widespread immunization coverage.
Case Studies: Comparing Vaccine Profiles
Case studies comparing vaccine profiles highlight the balance between efficacy and reactogenicity, emphasizing varying immune responses and side effects across populations. Data from mRNA and viral vector vaccines reveal high efficacy rates correlated with distinct reactogenicity patterns, such as localized pain or systemic symptoms. Understanding these differences informs tailored vaccination strategies optimizing protection while minimizing adverse reactions.
Patient Considerations and Risk Communication
Balancing vaccine efficacy and reactogenicity requires clear patient-centered communication to manage expectations about benefits and side effects. Transparent discussions emphasizing the likelihood and severity of potential adverse reactions enhance informed consent and trust. Tailoring risk communication to individual patient concerns supports shared decision-making and improves adherence to vaccination schedules.
Efficacy Infographic
 libterm.com
libterm.com