VIPoma is a rare neuroendocrine tumor that primarily secretes vasoactive intestinal peptide (VIP), leading to severe watery diarrhea, electrolyte imbalances, and dehydration. Early diagnosis and targeted treatment are crucial to manage symptoms and improve quality of life. Discover how to recognize the signs and explore advanced therapeutic options in the rest of this article.
Table of Comparison
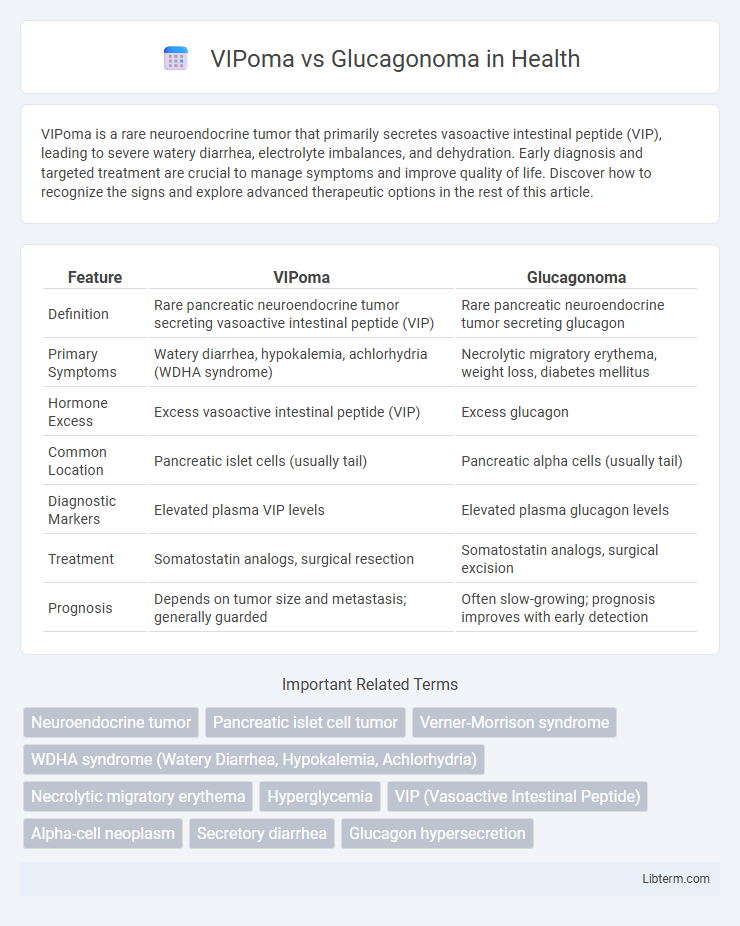
| Feature | VIPoma | Glucagonoma |
|---|---|---|
| Definition | Rare pancreatic neuroendocrine tumor secreting vasoactive intestinal peptide (VIP) | Rare pancreatic neuroendocrine tumor secreting glucagon |
| Primary Symptoms | Watery diarrhea, hypokalemia, achlorhydria (WDHA syndrome) | Necrolytic migratory erythema, weight loss, diabetes mellitus |
| Hormone Excess | Excess vasoactive intestinal peptide (VIP) | Excess glucagon |
| Common Location | Pancreatic islet cells (usually tail) | Pancreatic alpha cells (usually tail) |
| Diagnostic Markers | Elevated plasma VIP levels | Elevated plasma glucagon levels |
| Treatment | Somatostatin analogs, surgical resection | Somatostatin analogs, surgical excision |
| Prognosis | Depends on tumor size and metastasis; generally guarded | Often slow-growing; prognosis improves with early detection |
Introduction to VIPoma and Glucagonoma
VIPoma and Glucagonoma are rare neuroendocrine tumors originating from the pancreas, characterized by distinct hormone secretions affecting metabolism and electrolyte balance. VIPomas secrete vasoactive intestinal peptide (VIP), leading to severe watery diarrhea, hypokalemia, and achlorhydria, while Glucagonomas produce excess glucagon, causing hyperglycemia, weight loss, and characteristic necrolytic migratory erythema. Both tumors require precise biochemical testing and imaging for diagnosis due to their overlapping but specific clinical presentations.
Epidemiology and Prevalence
VIPomas and glucagonomas are rare neuroendocrine tumors with distinct epidemiological profiles; VIPomas have an incidence of approximately 0.2-0.5 cases per million annually, while glucagonomas occur slightly less frequently, around 0.01-0.1 cases per million per year. Both tumors predominantly affect adults between 30 and 60 years of age, with a slight female predominance reported in glucagonoma cases. Geographic and demographic variations are minimal, but early diagnosis remains challenging due to their rarity and nonspecific clinical presentations.
Pathophysiology and Hormonal Activity
VIPoma arises from pancreatic islet cells producing excessive vasoactive intestinal peptide (VIP), leading to severe watery diarrhea, hypokalemia, and achlorhydria by stimulating intestinal secretion and inhibiting gastric acid. In contrast, Glucagonoma originates from alpha cells of the pancreas, secreting excess glucagon, which causes hyperglycemia, weight loss, and necrolytic migratory erythema due to increased gluconeogenesis and lipolysis. Both neuroendocrine tumors disrupt normal hormonal regulation but differ distinctly in their secreted peptides and resulting systemic effects.
Clinical Presentation and Symptoms
VIPoma presents with watery diarrhea, hypokalemia, and achlorhydria, collectively known as WDHA syndrome, along with dehydration and muscle weakness, while glucagonoma typically manifests as necrolytic migratory erythema, new-onset diabetes mellitus, weight loss, and anemia. Both tumors arise from pancreatic islet cells but secrete different hormones--vasoactive intestinal peptide (VIP) in VIPoma and glucagon in glucagonoma--leading to distinct clinical features. Early recognition of these symptom complexes is essential for accurate diagnosis and targeted treatment.
Diagnostic Criteria and Laboratory Findings
VIPoma diagnosis relies on elevated vasoactive intestinal peptide (VIP) levels typically above 75 pg/mL, accompanied by watery diarrhea, hypokalemia, and achlorhydria. Glucagonoma is identified by markedly increased plasma glucagon concentrations, often exceeding 500 pg/mL, and clinical features such as necrolytic migratory erythema and hyperglycemia. Imaging studies, including somatostatin receptor scintigraphy or endoscopic ultrasound, assist in localizing pancreatic neuroendocrine tumors in both conditions.
Imaging Studies and Localization
VIPoma and Glucagonoma are rare neuroendocrine tumors primarily localized through advanced imaging techniques such as contrast-enhanced CT and MRI, which provide high-resolution visualization of pancreatic lesions. Somatostatin receptor scintigraphy (SRS) and Ga-68 DOTATATE PET/CT are highly sensitive functional imaging modalities that facilitate precise tumor localization and detection of metastatic sites for both tumor types. Endoscopic ultrasound (EUS) offers detailed assessment and biopsy capability, crucial for confirming diagnosis and guiding surgical planning specifically within pancreatic VIPomas and Glucagonomas.
Differential Diagnosis
VIPoma and glucagonoma are rare neuroendocrine tumors differentiated primarily by their hormone secretion profiles and clinical presentations. VIPomas secrete vasoactive intestinal peptide causing watery diarrhea, hypokalemia, and achlorhydria (WDHA syndrome), whereas glucagonomas produce excess glucagon leading to hyperglycemia, weight loss, and necrolytic migratory erythema. Laboratory tests showing elevated vasoactive intestinal peptide versus glucagon levels, combined with imaging studies locating pancreatic neuroendocrine tumors, are crucial for accurate differential diagnosis and tailored treatment approaches.
Treatment Modalities
Treatment modalities for VIPoma primarily include surgical resection of the pancreatic tumor, supported by somatostatin analogs like octreotide to control severe watery diarrhea and electrolyte imbalances. Glucagonoma treatment centers on tumor removal combined with somatostatin analogs to reduce glucagon secretion and alleviate necrolytic migratory erythema, weight loss, and hyperglycemia. Both neuroendocrine tumors may require targeted therapies such as everolimus or peptide receptor radionuclide therapy (PRRT) for metastatic or unresectable disease.
Prognosis and Outcomes
VIPoma generally has a more favorable prognosis with appropriate somatostatin analog therapy and surgical resection, though metastatic disease can worsen outcomes significantly. Glucagonoma prognosis depends strongly on early detection; tumor resection can be curative, but advanced disease with metastases often leads to poor survival rates. Both tumors are rare neuroendocrine neoplasms with variable clinical courses influenced by tumor burden and response to targeted treatments.
Key Differences Between VIPoma and Glucagonoma
VIPoma primarily secretes vasoactive intestinal peptide causing severe watery diarrhea, hypokalemia, and achlorhydria, while glucagonoma is characterized by excessive glucagon release leading to hyperglycemia, weight loss, and necrolytic migratory erythema. VIPoma tumors often originate in the pancreatic delta cells, whereas glucagonomas arise from pancreatic alpha cells. Diagnostic differentiation includes elevated VIP levels in VIPoma and increased glucagon levels in glucagonoma, with imaging techniques such as CT and MRI used for tumor localization.
VIPoma Infographic
 libterm.com
libterm.com