Dysesthesia is a condition characterized by abnormal and often unpleasant sensations such as burning, tingling, or numbness caused by nerve damage or dysfunction. It can affect various parts of the body and significantly impact daily comfort and mobility. Explore the rest of the article to understand the causes, symptoms, and treatment options for managing dysesthesia effectively.
Table of Comparison
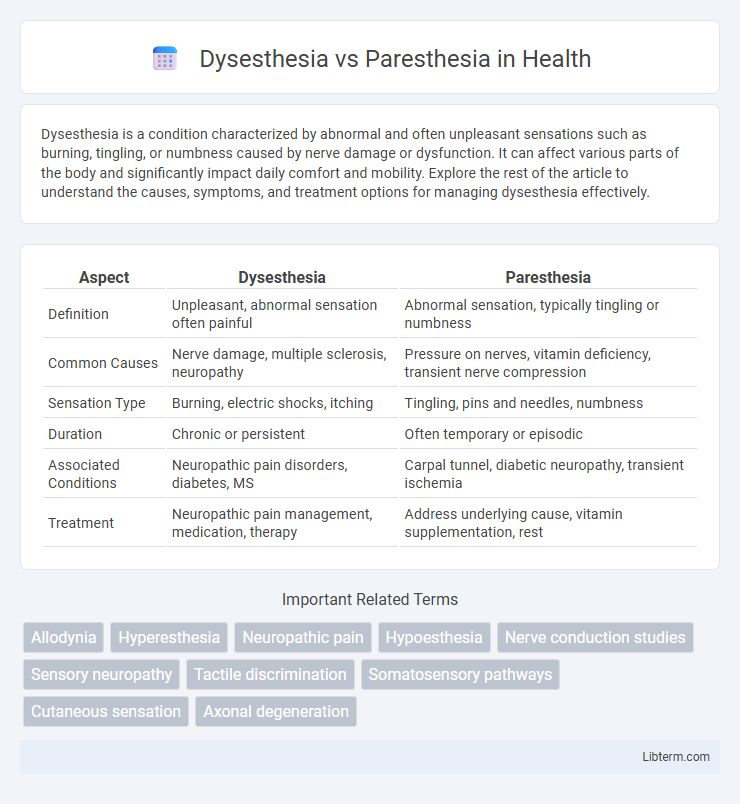
| Aspect | Dysesthesia | Paresthesia |
|---|---|---|
| Definition | Unpleasant, abnormal sensation often painful | Abnormal sensation, typically tingling or numbness |
| Common Causes | Nerve damage, multiple sclerosis, neuropathy | Pressure on nerves, vitamin deficiency, transient nerve compression |
| Sensation Type | Burning, electric shocks, itching | Tingling, pins and needles, numbness |
| Duration | Chronic or persistent | Often temporary or episodic |
| Associated Conditions | Neuropathic pain disorders, diabetes, MS | Carpal tunnel, diabetic neuropathy, transient ischemia |
| Treatment | Neuropathic pain management, medication, therapy | Address underlying cause, vitamin supplementation, rest |
Understanding Dysesthesia: Definition and Symptoms
Dysesthesia is a neurological condition characterized by abnormal, often unpleasant sensations such as burning, itching, or electric shock-like feelings, frequently resulting from nerve damage or dysfunction. Unlike paresthesia, which involves harmless tingling or numbness, dysesthesia sensations are typically painful and disruptive. Common symptoms include persistent burning pain, hypersensitivity to touch, and spontaneous discomfort without external stimuli, often seen in conditions like multiple sclerosis and diabetic neuropathy.
What is Paresthesia? Key Characteristics
Paresthesia is a neurological condition characterized by abnormal sensations such as tingling, prickling, or numbness, often described as "pins and needles." It typically results from nerve damage, compression, or irritation affecting sensory pathways, leading to spontaneous, non-painful sensory disturbances. Common causes include peripheral neuropathy, diabetes, multiple sclerosis, and temporary nerve compression like sitting cross-legged for extended periods.
Dysesthesia vs Paresthesia: Core Differences
Dysesthesia refers to unpleasant, abnormal sensations such as burning, electric, or aching pain often triggered by light touch, whereas paresthesia involves abnormal sensations like tingling, numbness, or prickling without necessarily being painful. Dysesthesia typically indicates nerve damage or dysfunction resulting in distorted sensory perception, while paresthesia can be transient or chronic and is often linked to temporary nerve irritation. Understanding these core differences is essential for accurate diagnosis and targeted neurological treatment.
Common Causes of Dysesthesia
Dysesthesia commonly results from nerve damage due to conditions such as diabetes mellitus, multiple sclerosis, and peripheral neuropathy, causing abnormal sensations like burning or electric shocks. Other causes include chemotherapy-induced nerve injury, spinal cord trauma, and post-herpetic neuralgia, which disrupt normal sensory processing. Unlike paresthesia, which often involves tingling or numbness without pain, dysesthesia is characterized by unpleasant or painful sensations triggered by stimuli that are normally non-painful.
Common Causes of Paresthesia
Paresthesia commonly arises from nerve compression, repetitive strain injuries, diabetes mellitus, and peripheral neuropathy, which disrupt normal sensory nerve function. Other frequent causes include vitamin deficiencies (such as B12), multiple sclerosis, and infections like shingles. Understanding these etiologies helps differentiate paresthesia, characterized by tingling or numbness, from dysesthesia, which involves unpleasant or painful sensations.
Diagnostic Approaches: Differentiating the Conditions
Diagnostic approaches for dysesthesia and paresthesia rely heavily on patient history and clinical examination, with sensory testing playing a pivotal role in differentiating the conditions. Electrophysiological studies, such as nerve conduction velocity (NCV) and electromyography (EMG), help identify nerve damage patterns, while imaging techniques like MRI can detect underlying structural causes. Quantitative sensory testing (QST) provides objective data on sensory nerve function, enabling more precise distinction between dysesthetic pain and non-painful paresthetic sensations.
Treatment Options for Dysesthesia
Treatment options for dysesthesia primarily include medications such as anticonvulsants, antidepressants, and topical agents like lidocaine to manage abnormal sensations. Physical therapy and sensory re-education techniques are often employed to improve nerve function and reduce discomfort. In severe cases, interventions like nerve blocks or spinal cord stimulation may be considered to alleviate persistent symptoms.
Managing and Treating Paresthesia
Paresthesia management primarily involves addressing the underlying cause, such as nerve compression, diabetes, or vitamin deficiencies, to reduce symptom severity. Treatment options include medications like anticonvulsants, antidepressants, and topical agents that modulate nerve signals and alleviate abnormal sensations. Physical therapy, lifestyle modifications, and in some cases surgical intervention may be necessary to improve nerve function and prevent symptom progression.
When to Seek Medical Attention
Seek medical attention for dysesthesia if experiencing persistent burning pain, electric shock sensations, or severe discomfort disrupting daily activities, as it may indicate nerve damage or underlying neurological disorders. In cases of paresthesia, urgent evaluation is necessary when numbness or tingling occurs suddenly, worsens rapidly, or is accompanied by weakness, dizziness, or loss of coordination, signaling potential stroke or acute nerve injury. Chronic or unexplained sensory disturbances warrant professional assessment to determine cause and appropriate treatment to prevent long-term complications.
Preventive Measures and Lifestyle Tips
Dysesthesia and paresthesia can be managed and sometimes prevented by maintaining proper ergonomic practices and avoiding repetitive strain injuries. Incorporating regular breaks during activities and using supportive devices helps reduce nerve compression that leads to abnormal sensations. Ensuring a balanced diet rich in B vitamins and controlling underlying conditions like diabetes significantly lowers the risk of nerve damage associated with these sensory disorders.
Dysesthesia Infographic
 libterm.com
libterm.com