Dysphagia, characterized by difficulty swallowing, can result from various medical conditions affecting the throat or esophagus. Early diagnosis and targeted treatment are crucial to prevent complications such as malnutrition or aspiration pneumonia. Discover how you can recognize the symptoms and explore effective management strategies in the rest of this article.
Table of Comparison
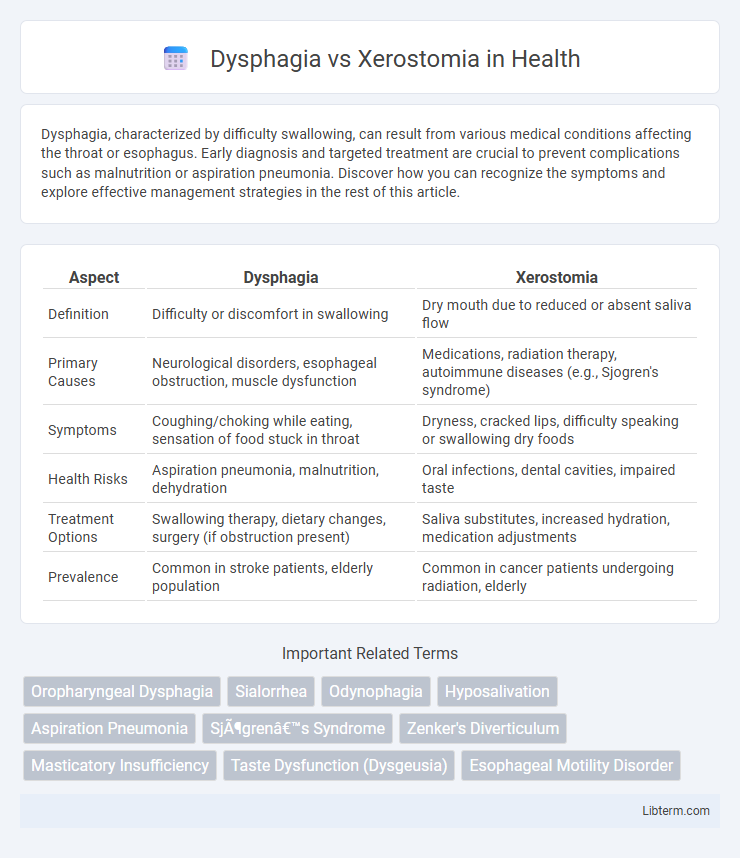
| Aspect | Dysphagia | Xerostomia |
|---|---|---|
| Definition | Difficulty or discomfort in swallowing | Dry mouth due to reduced or absent saliva flow |
| Primary Causes | Neurological disorders, esophageal obstruction, muscle dysfunction | Medications, radiation therapy, autoimmune diseases (e.g., Sjogren's syndrome) |
| Symptoms | Coughing/choking while eating, sensation of food stuck in throat | Dryness, cracked lips, difficulty speaking or swallowing dry foods |
| Health Risks | Aspiration pneumonia, malnutrition, dehydration | Oral infections, dental cavities, impaired taste |
| Treatment Options | Swallowing therapy, dietary changes, surgery (if obstruction present) | Saliva substitutes, increased hydration, medication adjustments |
| Prevalence | Common in stroke patients, elderly population | Common in cancer patients undergoing radiation, elderly |
Understanding Dysphagia: Definition and Causes
Dysphagia is a medical condition characterized by difficulty in swallowing due to abnormalities in the muscles or nerves involved in the swallowing process. Common causes include neurological disorders such as stroke, Parkinson's disease, and multiple sclerosis, as well as structural abnormalities like esophageal strictures or tumors. Understanding the underlying cause of dysphagia is crucial for effective treatment and management, differentiating it from xerostomia, which primarily involves dry mouth due to reduced saliva production.
Unpacking Xerostomia: What Is Dry Mouth?
Xerostomia, commonly known as dry mouth, occurs due to decreased saliva production, impacting oral health and digestion. Unlike dysphagia, which refers to difficulty swallowing, xerostomia primarily causes discomfort, increased risk of tooth decay, and speech challenges. Understanding xerostomia involves recognizing its symptoms, causes such as medication side effects or autoimmune diseases, and appropriate treatments to restore saliva flow.
Key Differences Between Dysphagia and Xerostomia
Dysphagia is a medical condition characterized by difficulty swallowing, often caused by neurological disorders, muscle abnormalities, or structural blockages in the throat or esophagus, whereas xerostomia refers to dry mouth resulting from reduced or absent saliva flow, commonly due to medication side effects or autoimmune diseases. Dysphagia primarily affects the swallowing mechanism and can lead to aspiration pneumonia or malnutrition, while xerostomia impacts oral health by increasing the risk of tooth decay, oral infections, and impaired chewing or speech. Diagnostic evaluations for dysphagia often include videofluoroscopic swallowing studies or endoscopy, whereas xerostomia diagnosis primarily relies on patient history, salivary flow tests, and clinical examination.
Common Symptoms: How Dysphagia and Xerostomia Present
Dysphagia presents with difficulty swallowing, sensation of food sticking in the throat, and coughing or choking during meals, often leading to weight loss and malnutrition. Xerostomia is characterized by a dry mouth, thick saliva, altered taste, and difficulty speaking or swallowing due to reduced saliva production. Both conditions impact oral intake but differ in their primary symptoms and underlying causes.
Underlying Risk Factors for Dysphagia and Xerostomia
Dysphagia, characterized by difficulty swallowing, often results from neurological conditions such as stroke, Parkinson's disease, or multiple sclerosis, as well as structural abnormalities in the esophagus. Xerostomia, or dry mouth, primarily arises from salivary gland dysfunction due to medications like anticholinergics, radiation therapy for head and neck cancer, or systemic diseases such as Sjogren's syndrome. Both conditions share overlapping risk factors including advanced age and polypharmacy, which exacerbate oral and pharyngeal function impairments.
Diagnosis: How Doctors Identify Each Condition
Doctors diagnose dysphagia through comprehensive clinical evaluations including swallowing studies such as videofluoroscopic swallow examination and fiberoptic endoscopic evaluation of swallowing (FEES), assessing the mechanics of swallowing and identifying structural or neurological impairments. Xerostomia diagnosis relies on patient symptoms of dry mouth, complemented by sialometry to measure saliva flow rates and clinical examination to detect mucosal dryness or oral lesions. Advanced imaging or biopsy may be utilized for underlying causes in both conditions but remain secondary to primary functional assessments.
Impact on Nutrition and Quality of Life
Dysphagia severely impairs swallowing, leading to inadequate nutrient intake and increased risk of malnutrition and aspiration pneumonia, which drastically reduces quality of life. Xerostomia, characterized by dry mouth due to reduced saliva flow, hampers chewing and swallowing, causing difficulty in tasting food and resulting in decreased appetite and nutritional deficiencies. Both conditions significantly compromise oral intake, necessitating tailored dietary modifications and multidisciplinary interventions to enhance patient well-being and nutritional status.
Treatment Options for Dysphagia vs Xerostomia
Treatment options for dysphagia primarily include swallowing therapy, dietary modifications, and in severe cases, surgical interventions or feeding tube placement to ensure adequate nutrition. Xerostomia management focuses on stimulating saliva production through medications like pilocarpine, saliva substitutes, and maintaining hydration to alleviate dry mouth symptoms. Both conditions benefit from interdisciplinary care involving speech therapists, dentists, and medical specialists to optimize patient outcomes.
Prevention Strategies and Lifestyle Modifications
Effective prevention strategies for dysphagia include maintaining good oral hygiene, performing swallowing exercises, and managing underlying neurological or muscular conditions. For xerostomia, lifestyle modifications such as staying hydrated, avoiding alcohol and caffeine, and using saliva substitutes can significantly reduce symptoms. Both conditions benefit from regular medical evaluations and dietary adjustments to enhance oral function and comfort.
When to Seek Medical Advice for Swallowing or Dry Mouth Issues
Seek medical advice for dysphagia if you experience persistent difficulty swallowing, choking, coughing during meals, or unexplained weight loss, as these symptoms may indicate underlying neurological or esophageal disorders. For xerostomia, consult a healthcare provider if dry mouth is chronic, causes difficulty speaking, chewing, or swallowing, or leads to increased dental decay and oral infections. Early evaluation by a speech therapist, dentist, or specialist helps prevent complications and improves management of both swallowing and salivary gland dysfunction.
Dysphagia Infographic
 libterm.com
libterm.com