Diverticulitis is a digestive condition characterized by inflammation or infection of small pouches called diverticula that develop along the walls of your colon. Symptoms often include abdominal pain, fever, and changes in bowel habits, potentially leading to serious complications if untreated. Discover more about causes, treatments, and preventive measures to protect your digestive health by reading the full article.
Table of Comparison
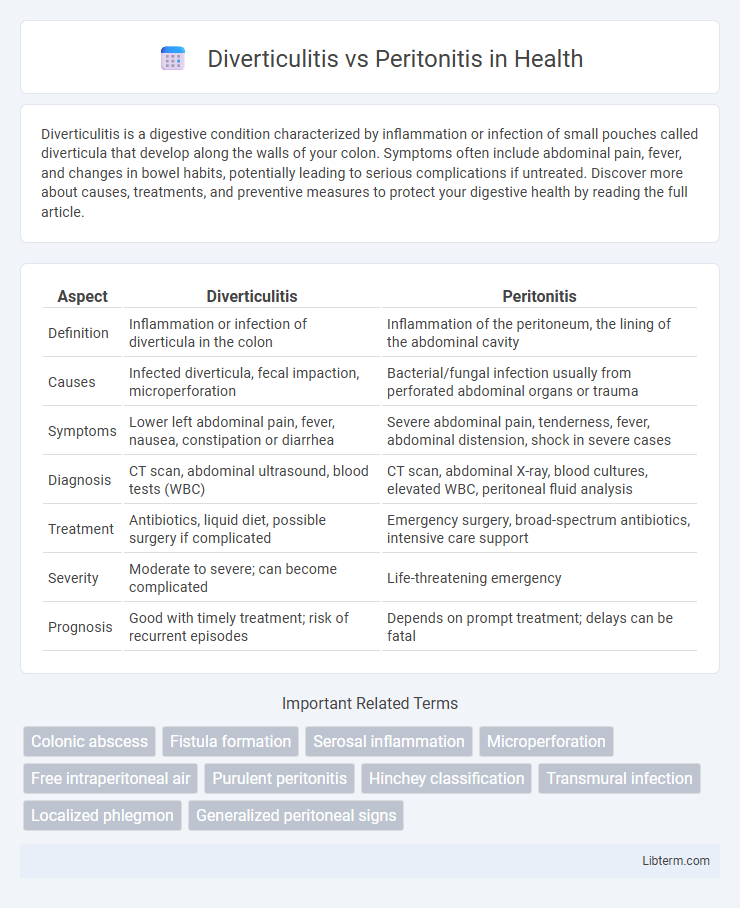
| Aspect | Diverticulitis | Peritonitis |
|---|---|---|
| Definition | Inflammation or infection of diverticula in the colon | Inflammation of the peritoneum, the lining of the abdominal cavity |
| Causes | Infected diverticula, fecal impaction, microperforation | Bacterial/fungal infection usually from perforated abdominal organs or trauma |
| Symptoms | Lower left abdominal pain, fever, nausea, constipation or diarrhea | Severe abdominal pain, tenderness, fever, abdominal distension, shock in severe cases |
| Diagnosis | CT scan, abdominal ultrasound, blood tests (WBC) | CT scan, abdominal X-ray, blood cultures, elevated WBC, peritoneal fluid analysis |
| Treatment | Antibiotics, liquid diet, possible surgery if complicated | Emergency surgery, broad-spectrum antibiotics, intensive care support |
| Severity | Moderate to severe; can become complicated | Life-threatening emergency |
| Prognosis | Good with timely treatment; risk of recurrent episodes | Depends on prompt treatment; delays can be fatal |
Introduction to Diverticulitis and Peritonitis
Diverticulitis is an inflammation or infection of small pouches called diverticula that form in the walls of the colon, often causing abdominal pain, fever, and changes in bowel habits. Peritonitis is a serious inflammation of the peritoneum, the thin tissue lining the abdominal cavity, usually resulting from infection following a rupture in the gastrointestinal tract. Both conditions require prompt medical attention, but diverticulitis primarily affects the colon, whereas peritonitis involves widespread infection in the abdominal cavity.
Understanding Diverticulitis: Causes and Risk Factors
Diverticulitis occurs when small pouches called diverticula in the colon become inflamed or infected, often due to trapped stool or bacteria. Key risk factors include aging, low-fiber diet, obesity, smoking, and lack of physical activity, which increase the likelihood of diverticula formation and subsequent inflammation. Understanding these causes helps differentiate diverticulitis from peritonitis, a more severe inflammation of the peritoneum usually resulting from infection or abdominal injury.
Peritonitis Overview: Etiology and Risk Factors
Peritonitis is an inflammation of the peritoneum, often caused by bacterial or fungal infection due to perforation of abdominal organs, such as in cases of ruptured diverticulitis, appendicitis, or stomach ulcers. Risk factors include abdominal surgery, trauma, immunosuppression, liver disease with ascites, and peritoneal dialysis, which increase susceptibility to infection and peritoneal contamination. Early recognition and treatment are critical to prevent sepsis and multi-organ failure in patients with peritonitis.
Key Symptoms: Diverticulitis vs Peritonitis
Diverticulitis primarily presents with localized lower left abdominal pain, fever, and changes in bowel habits such as constipation or diarrhea. Peritonitis features more severe symptoms including widespread abdominal pain, tenderness, rigidity, and signs of systemic infection like high fever and rapid heart rate. Both conditions require prompt medical evaluation, as diverticulitis can progress to peritonitis if a diverticular rupture occurs.
Pathophysiology: How Each Condition Develops
Diverticulitis develops from the inflammation or infection of diverticula, small pouches that form in the colon wall due to increased intraluminal pressure and weakened colonic musculature. Peritonitis arises from the inflammation of the peritoneum, often triggered by bacterial infection following the perforation of abdominal organs, including ruptured diverticula. The pathophysiology of diverticulitis involves localized mucosal breach and bacterial invasion, whereas peritonitis involves a systemic inflammatory response due to widespread peritoneal contamination.
Diagnostic Approaches for Diverticulitis and Peritonitis
Diagnostic approaches for diverticulitis primarily involve abdominal CT scans with contrast, which provide detailed images to identify inflamed or infected diverticula and assess complications such as abscesses. For peritonitis, diagnosis relies on physical examination for signs of abdominal rigidity and tenderness, laboratory tests indicating elevated white blood cell count, and imaging techniques like abdominal X-rays or ultrasounds to detect free air or fluid suggesting peritoneal inflammation. Blood cultures and peritoneal fluid analysis obtained by paracentesis are critical in confirming peritonitis and guiding antimicrobial therapy.
Treatment Options: Medications, Surgery, and Aftercare
Treatment options for diverticulitis typically include antibiotics such as ciprofloxacin and metronidazole to address infection, with pain management using acetaminophen; severe cases may require surgical intervention like sigmoid colectomy. Peritonitis treatment demands prompt administration of broad-spectrum intravenous antibiotics such as piperacillin-tazobactam combined with emergency surgery to remove the source of infection and thorough peritoneal lavage. Aftercare for both conditions involves monitoring for complications, dietary adjustments, and follow-up imaging studies to ensure resolution and prevent recurrence.
Complications and Prognosis Comparison
Diverticulitis complications include abscess formation, fistulas, bowel obstruction, and perforation, which may lead to localized peritonitis. Peritonitis, often secondary to gastrointestinal perforation, can cause widespread infection, sepsis, and multi-organ failure if untreated. Prognosis for diverticulitis is generally favorable with appropriate antibiotic therapy, whereas peritonitis carries a higher morbidity and mortality risk, requiring prompt surgical intervention and intensive care.
Preventive Strategies for Both Conditions
Preventive strategies for diverticulitis include a high-fiber diet rich in fruits, vegetables, and whole grains to promote regular bowel movements and reduce colon pressure. For peritonitis, preventing infections through proper wound care, timely treatment of abdominal infections, and maintaining sterile techniques during surgeries is crucial. Regular medical check-ups to manage underlying conditions like diverticulosis or appendicitis also help minimize the risk of both diverticulitis and peritonitis.
When to Seek Immediate Medical Attention
Severe abdominal pain, persistent fever above 101degF (38.3degC), and signs of shock like rapid heartbeat or low blood pressure indicate the need for immediate medical attention in cases of diverticulitis and peritonitis. Sudden worsening of symptoms, including intense tenderness, bloating, or inability to pass gas or stool, suggests possible complications such as perforation or widespread infection requiring urgent care. Prompt diagnosis and treatment are critical to prevent life-threatening outcomes in both diverticulitis and peritonitis.
Diverticulitis Infographic
 libterm.com
libterm.com