Leukopenia is a condition characterized by a reduced white blood cell count, which impairs your immune system's ability to fight infections effectively. It can result from various factors including infections, medications, autoimmune disorders, or bone marrow problems. Discover the causes, symptoms, and treatments for leukopenia to better understand how it impacts your health.
Table of Comparison
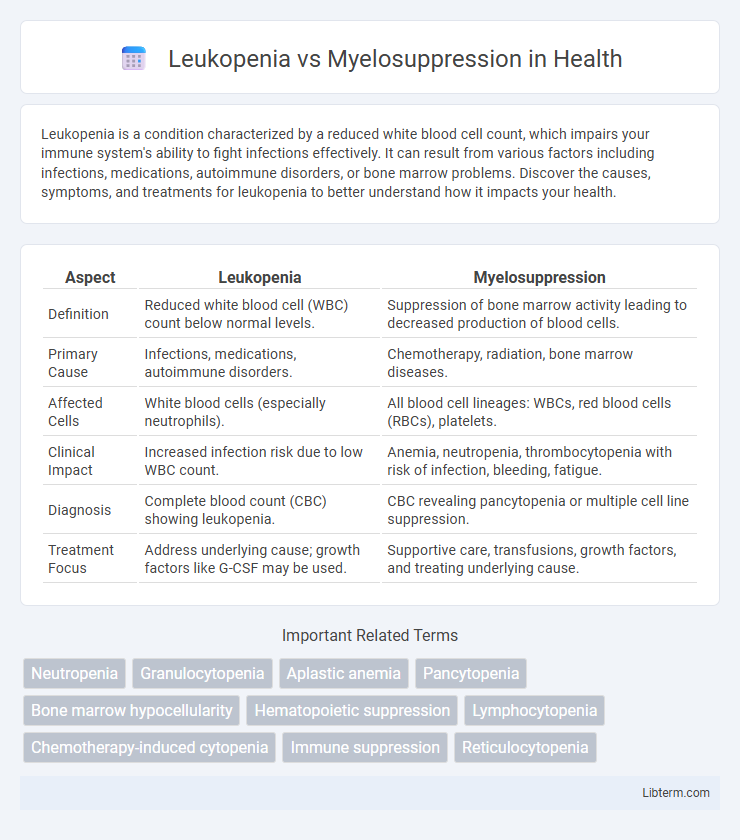
| Aspect | Leukopenia | Myelosuppression |
|---|---|---|
| Definition | Reduced white blood cell (WBC) count below normal levels. | Suppression of bone marrow activity leading to decreased production of blood cells. |
| Primary Cause | Infections, medications, autoimmune disorders. | Chemotherapy, radiation, bone marrow diseases. |
| Affected Cells | White blood cells (especially neutrophils). | All blood cell lineages: WBCs, red blood cells (RBCs), platelets. |
| Clinical Impact | Increased infection risk due to low WBC count. | Anemia, neutropenia, thrombocytopenia with risk of infection, bleeding, fatigue. |
| Diagnosis | Complete blood count (CBC) showing leukopenia. | CBC revealing pancytopenia or multiple cell line suppression. |
| Treatment Focus | Address underlying cause; growth factors like G-CSF may be used. | Supportive care, transfusions, growth factors, and treating underlying cause. |
Introduction to Leukopenia and Myelosuppression
Leukopenia is a condition characterized by an abnormally low white blood cell (WBC) count, which impairs the immune system's ability to fight infections. Myelosuppression refers to the decreased production of blood cells, including white blood cells, red blood cells, and platelets, due to bone marrow suppression often caused by chemotherapy or radiation therapy. Understanding the distinction between leukopenia as a specific reduction in WBCs and myelosuppression as a broader hematopoietic suppression is critical for clinical diagnosis and treatment planning.
Defining Leukopenia: Key Characteristics
Leukopenia is characterized by a reduction in white blood cell (WBC) count, specifically targeting neutrophils, which play a crucial role in fighting infections. It differs from myelosuppression, which broadly refers to the decreased bone marrow activity resulting in reduced production of multiple blood components, including red cells, white cells, and platelets. Key diagnostic markers for leukopenia include absolute neutrophil count (ANC) below 1,500 cells/uL, highlighting its impact on immune system vulnerability.
Understanding Myelosuppression: Overview
Myelosuppression is a condition characterized by the decreased production of blood cells due to bone marrow dysfunction, often caused by chemotherapy, radiation, or certain infections. This suppression leads to leukopenia, a specific reduction in white blood cells, increasing the risk of infections. Monitoring blood cell counts is critical in managing myelosuppression to prevent complications associated with immune deficiency and anemia.
Causes of Leukopenia
Leukopenia primarily results from infections, autoimmune diseases, bone marrow disorders, and the use of certain medications such as chemotherapy and immunosuppressants. Myelosuppression, a broader condition, involves the bone marrow's decreased ability to produce blood cells, which can lead to leukopenia among other cytopenias. Understanding the specific cause of leukopenia is crucial for targeted treatment and differentiating it from myelosuppression-related cytopenias.
Causes of Myelosuppression
Myelosuppression primarily results from chemotherapy drugs, radiation therapy, and certain bone marrow diseases, leading to decreased production of blood cells, including white blood cells, red blood cells, and platelets. Infections, autoimmune disorders, and toxic exposure to chemicals such as benzene can also contribute to bone marrow suppression. Unlike leukopenia, which specifically denotes a reduction in white blood cells, myelosuppression involves a broader impairment of the marrow's hematopoietic function.
Symptoms and Clinical Manifestations
Leukopenia is characterized by a significant reduction in white blood cells, leading to increased susceptibility to infections, frequent fevers, and sore throat, while myelosuppression involves the broader suppression of bone marrow activity, causing pancytopenia with symptoms such as anemia-induced fatigue, bleeding tendencies due to low platelets, and recurrent infections. Clinical manifestations of leukopenia primarily revolve around neutropenia and infections, whereas myelosuppression presents with multi-lineage cytopenias, including leukopenia, thrombocytopenia, and anemia. Monitoring blood counts and identifying underlying causes are critical for diagnosing and managing these hematologic conditions effectively.
Diagnostic Approaches
Leukopenia diagnosis involves complete blood count (CBC) analysis to identify reduced white blood cell levels, often followed by differential count and bone marrow biopsy to determine underlying causes. Myelosuppression diagnosis requires assessing bone marrow function through CBC, reticulocyte count, and bone marrow biopsy to detect decreased production of all blood cell lines. Advanced diagnostic tools like flow cytometry and cytogenetic analysis help differentiate between leukopenia due to peripheral destruction and myelosuppression caused by marrow failure.
Treatment Strategies
Leukopenia treatment strategies involve addressing the underlying cause and may include administration of granulocyte colony-stimulating factor (G-CSF) to stimulate white blood cell production. Myelosuppression management requires dose adjustment or interruption of chemotherapy agents, along with supportive care such as transfusions and growth factors to promote bone marrow recovery. Both conditions benefit from infection prophylaxis and close monitoring of blood counts to prevent complications.
Prognosis and Complications
Leukopenia, characterized by a decreased white blood cell count, generally has a better prognosis when promptly identified and managed, though it increases vulnerability to infections and sepsis. Myelosuppression, involving the broader suppression of bone marrow activity affecting all blood cell lines, carries a higher risk of severe complications such as anemia, bleeding, and life-threatening infections due to pancytopenia. Prognosis in myelosuppression often depends on the underlying cause and the effectiveness of interventions to restore marrow function or address toxic exposures.
Prevention and Patient Management Tips
Leukopenia prevention involves maintaining a healthy immune system through proper nutrition, infection control, and avoiding exposure to toxins, while myelosuppression management requires regular blood count monitoring and prompt treatment of infections or anemia. Patients undergoing chemotherapy or radiation should adhere to prescribed medications, report any signs of infection immediately, and practice good hygiene to reduce complications. Effective patient management includes individualized care plans, supportive therapies like growth factors, and patient education on symptom recognition and lifestyle adjustments to minimize risk.
Leukopenia Infographic
 libterm.com
libterm.com